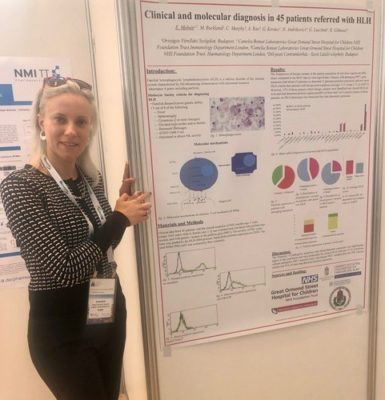
A clinical investigation on the key diagnostic markers for Autoimmune Lymphoproliferative Syndrome (ALPS) was published in Blood, one of the world’s most prestigious journals of immunology, the official journal of the American Society of Hematology. The first author of this publication is Dr. Emese Molnár, a young researcher, former student of medicine at Semmelweis University and currently a PhD doctoral candidate. Her determination and commitment have taken her from the Serbian town, Zenta to Great Ormond Street Hospital (GOSH) in London to pursue her dreams as a researcher and beyond.
When ambition meets talent
 As early as her high school years, Dr. Emese Molnár knew that she wanted to become a researcher and has done everything in her power to reach her goals. After graduating as a Doctor of Medicine at the Faculty of Medicine of Semmelweis University, she continued her education at the department of stem cell transplantation, which gave her an insight on cell therapies. However, solely her enthusiasm for haematology would not have set her on a path leading to a promising cooperation with Great Ormond Street Hospital (GOSH). It was the coincidence of a number of circumstances that made her seriously think about opening up new horizons in Hungarian gene and cell therapy; the tragic loss of a loved one to untreated lymphoma, her admission to the PhD programme at the department of stem cell transplantation and receiving a rising star award at an international conference in the US.
As early as her high school years, Dr. Emese Molnár knew that she wanted to become a researcher and has done everything in her power to reach her goals. After graduating as a Doctor of Medicine at the Faculty of Medicine of Semmelweis University, she continued her education at the department of stem cell transplantation, which gave her an insight on cell therapies. However, solely her enthusiasm for haematology would not have set her on a path leading to a promising cooperation with Great Ormond Street Hospital (GOSH). It was the coincidence of a number of circumstances that made her seriously think about opening up new horizons in Hungarian gene and cell therapy; the tragic loss of a loved one to untreated lymphoma, her admission to the PhD programme at the department of stem cell transplantation and receiving a rising star award at an international conference in the US.
Living and working in the land of CAR T-cell therapy
Her attention turned towards chimeric antigen receptor (CAR) T-cell therapy, a promising new method to get a type of immune cells, called T cells to fight lymphoma, leukaemia or other haematological cancers. The patient’s T-cells are collected and reprogrammed in a lab to specifically target tumour cells. These genetically altered T-cells (now CAR T-cells) are given back to the patient to launch a targeted attack on the cancer cells. Dr. Molnár was determined to learn the procedure and build relationships that may pave the way to the establishment of an institution providing gene therapy in Hungary. She applied for an Erasmus+ grant with the aim of finding a place for internship in the United Kingdom, the land of CAR T-cell therapy.
After a cursory visit and a casual meeting at a conference, she found herself holding the invitation letter of Great Ormond Street Hospital, which was the first institution in the United Kingdom to perform gene therapy. Her supervisor was Dr. Kimberly Gilmour, a clinical scientist and the head of the national service for diagnosing patients with primary immunodeficiencies. With her help, Dr. Molnár started to work as a member of the CAR T-cell immunotherapy group of University College London (UCL), where she spent part of her internship monitoring and treating CAR T patients, preparing patient portfolios and analysing lab results. In addition to treating and managing the platform containing all the CAR T-cell therapies in the UK, she spent the rest of her time working with patients with primary immunodeficiencies under the guidance of Dr. Gilmour. This was the part of her work that led to the publication of her study in Blood journal.
Breakthrough in diagnosing ALPS
 Autoimmune Lymphoproliferative Syndrome (ALPS) is a genetic disorder that is characterised by the production of abnormally large number of lymphocytes (immune cells). It is considered a rare disease, though it is hard to say how rare it is, as it is very difficult to diagnose. Symptoms may include enlarged lymph nodes, liver and spleen where lymphocytes accumulate in high numbers. These symptoms are overly generic and may suggest other conditions, such as infection, lymphoma or just an atypical manifestation of enlarged lymph nodes. The manifestation of the syndrome may be very diverse as well by being asymptomatic in some patients and causing debilitating condition in others. In addition, the appearance of the symptoms may occur at any time during the life of the patients. However, sooner or later the syndrome could turn into some kind of malignity even in asymptomatic patients. It was a known fact that in some patients with ALPS a gene that is linked to apoptosis is mutated. Apoptosis is a form of programmed cell death and if it is inhibited, it leads to unnatural cell accumulation. If the cells in the tumour are unable to die, immune cells will also be unable to destroy them, so chemotherapy is the only option for their elimination. That is why an effective and early diagnosis of ALPS is crucial.
Autoimmune Lymphoproliferative Syndrome (ALPS) is a genetic disorder that is characterised by the production of abnormally large number of lymphocytes (immune cells). It is considered a rare disease, though it is hard to say how rare it is, as it is very difficult to diagnose. Symptoms may include enlarged lymph nodes, liver and spleen where lymphocytes accumulate in high numbers. These symptoms are overly generic and may suggest other conditions, such as infection, lymphoma or just an atypical manifestation of enlarged lymph nodes. The manifestation of the syndrome may be very diverse as well by being asymptomatic in some patients and causing debilitating condition in others. In addition, the appearance of the symptoms may occur at any time during the life of the patients. However, sooner or later the syndrome could turn into some kind of malignity even in asymptomatic patients. It was a known fact that in some patients with ALPS a gene that is linked to apoptosis is mutated. Apoptosis is a form of programmed cell death and if it is inhibited, it leads to unnatural cell accumulation. If the cells in the tumour are unable to die, immune cells will also be unable to destroy them, so chemotherapy is the only option for their elimination. That is why an effective and early diagnosis of ALPS is crucial.
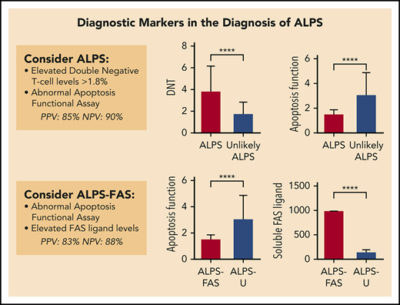 The clinical investigation was based on laboratory results and genetic analysis of patients who have been suspected of ALPS in the past 10 years. The study evaluated laboratory findings, clinical manifestations and molecular genetic results of the patients. In vitro apoptosis functional tests were performed to determine whether apoptosis is concluded in each and every blood sample. If cell death did not take place, they sought to determine where the pathway’s inhibition occurred. They were able to draw up a pattern that showed correlation among three parameters; excessive rate of lymphoproliferation (the production of an excessive number of immune cells), high percentage of double negative T-cells (type of white blood cell in the peripheral blood and lymphoid organs) and abnormal apoptosis. By using the combination of the above parameters clinicians can now easily and quickly diagnose patients with ALPS, while previously this was only possible by comparing 6-8 parameters. The study has amended the existing protocol and provided a functional aid to practising clinicians in the diagnosis of ALPS.
The clinical investigation was based on laboratory results and genetic analysis of patients who have been suspected of ALPS in the past 10 years. The study evaluated laboratory findings, clinical manifestations and molecular genetic results of the patients. In vitro apoptosis functional tests were performed to determine whether apoptosis is concluded in each and every blood sample. If cell death did not take place, they sought to determine where the pathway’s inhibition occurred. They were able to draw up a pattern that showed correlation among three parameters; excessive rate of lymphoproliferation (the production of an excessive number of immune cells), high percentage of double negative T-cells (type of white blood cell in the peripheral blood and lymphoid organs) and abnormal apoptosis. By using the combination of the above parameters clinicians can now easily and quickly diagnose patients with ALPS, while previously this was only possible by comparing 6-8 parameters. The study has amended the existing protocol and provided a functional aid to practising clinicians in the diagnosis of ALPS.
A dream to come true: gene therapy lab in Budapest
 The study of Dr. Emese Molnár published in Blood was not the only successful result of her internship at GOSH. Ever since she was a medical student she has been determined to set up a gene therapy lab at Semmelweis University and has been looking for ways to realise it. Now it seems her dream is about to come true in the form of a scientific cooperation between GOSH and UCL supported by the Hungarian Embassy in London and Semmelweis University’s Innovation Centre. The portfolio of the planned gene therapy lab would include CAR T-cell therapy for cancer patients, stem cell transplantation and treatment of children with primary immunodeficiencies. In addition to the application of the therapies already in use, the centre would provide a platform for the development, production and monitoring of new cellular and gene therapy products. Currently, gene and cell therapy targeting diverse diseases and syndromes are available only in the United Kingdom. Although, there are some clinical trials occasionally conducted in various parts of Europe, there is only one centre to refer European patients to. With the establishment of the gene therapy lab in Budapest, a regional centre of regenerative medicine would be set up, which fits in the biotechnological platform of Semmelweis University’s Health Industry-Biotechnology Science Park. The collaboration between GOSH and Semmelweis University will be mutually beneficial for both institutions; GOSH would contribute to the project by providing professional support and supervision in audits and authorization, while Semmelweis University would provide a stable European partnership and high quality clinical and scientific research.
The study of Dr. Emese Molnár published in Blood was not the only successful result of her internship at GOSH. Ever since she was a medical student she has been determined to set up a gene therapy lab at Semmelweis University and has been looking for ways to realise it. Now it seems her dream is about to come true in the form of a scientific cooperation between GOSH and UCL supported by the Hungarian Embassy in London and Semmelweis University’s Innovation Centre. The portfolio of the planned gene therapy lab would include CAR T-cell therapy for cancer patients, stem cell transplantation and treatment of children with primary immunodeficiencies. In addition to the application of the therapies already in use, the centre would provide a platform for the development, production and monitoring of new cellular and gene therapy products. Currently, gene and cell therapy targeting diverse diseases and syndromes are available only in the United Kingdom. Although, there are some clinical trials occasionally conducted in various parts of Europe, there is only one centre to refer European patients to. With the establishment of the gene therapy lab in Budapest, a regional centre of regenerative medicine would be set up, which fits in the biotechnological platform of Semmelweis University’s Health Industry-Biotechnology Science Park. The collaboration between GOSH and Semmelweis University will be mutually beneficial for both institutions; GOSH would contribute to the project by providing professional support and supervision in audits and authorization, while Semmelweis University would provide a stable European partnership and high quality clinical and scientific research.
While working on the realisation of the collaboration, Dr. Emese Molnár keeps on with her research on ALPS, is applying for a grant of the European Haematology Association for young researchers and is writing her doctoral dissertation. In the near future she plans to continue and conclude research on immunodeficiency and to get more active in a clinical collaboration between GOSH and Semmelweis University in the field of CAR T-cell therapy.
Ágnes Raubinek
Photo: Dr. Emese Molnár; Gábor Takács-Carvalho – Embassy of Hungary in London
Illustration: Blood publication