In Hungary, cancer remains one of the leading causes of death. According to data from the Hungarian Central Statistical Office, between 2010 and 2019, cancer was responsible for 32,000 to 34,000 deaths per year. In the same period, based on data from the National Cancer Registry managed by the National Institute of Oncology, the annual number of newly registered malignant diseases rose from 65,766 to 75,347 by 2019. At the same time, in the period between 2011 and 2019, cancer mortality data improved by 11 percent for men and 6 percent for women, according to this year’s announcement of the Hungarian League Against Cancer published on National Cancer Day.
These results can be accounted for the development of medicine, clinical care organization and molecular diagnostics, which together give impetus to the increasingly effective action against cancer diseases.
In line with this, since January 2022, with the support of the National Health Insurance Fund of Hungary (NEAK), comprehensive genetic profiling has also been available for adult patients who are less responsive to standard protocols or who do not respond at all.
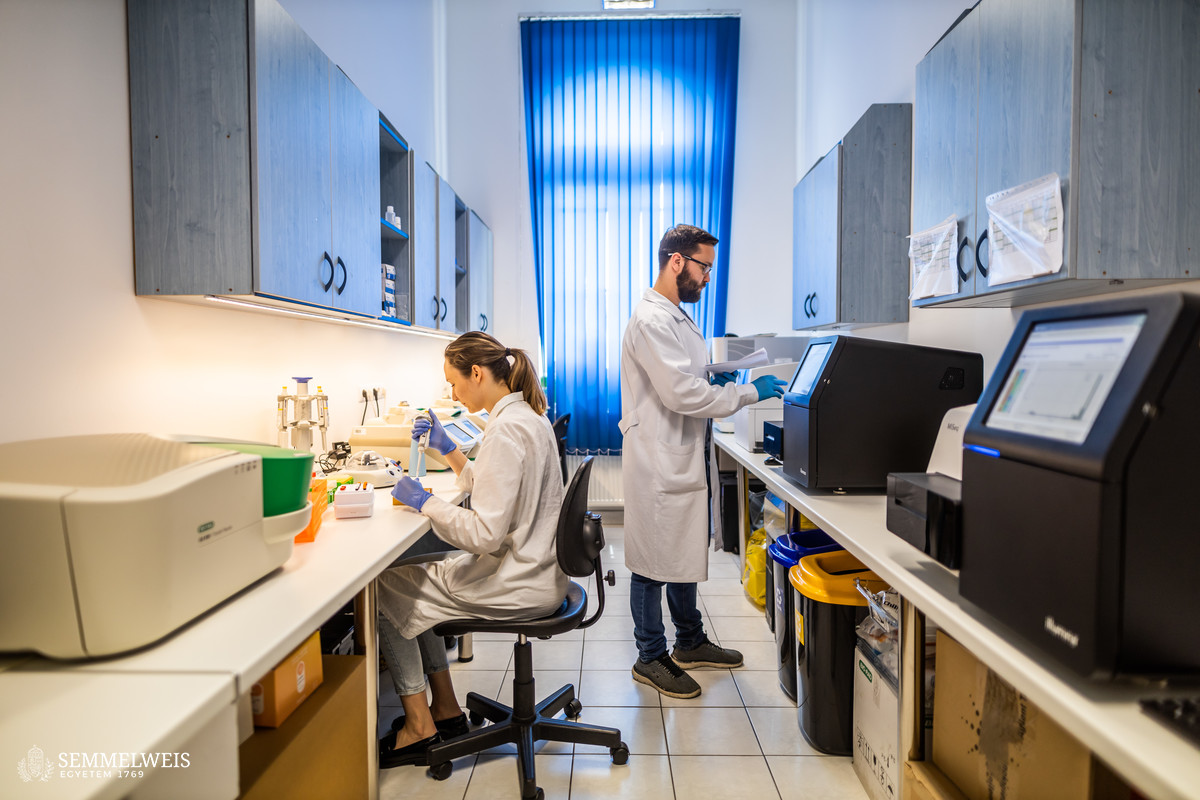
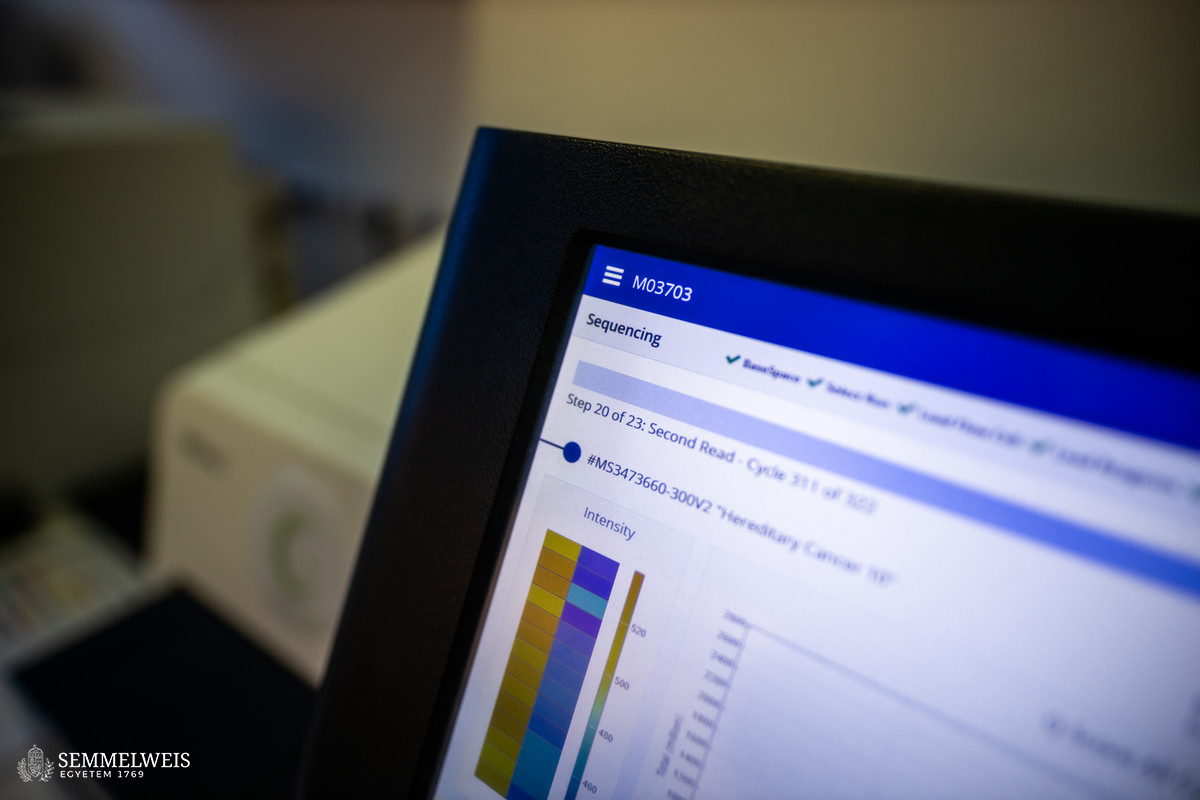
 “Like in pediatric oncology, the main goal in the case of adult patients is to identify new therapeutic targets, which is currently possible by a next-generation sequencing examination focusing on more than 500 genes, performed with a new-generation sequencer (Illumina, Trusight Oncology 500). The NEAK committee, which meets weekly, decides on the state financing of this at the initiative of the attending physicians,” said Semmelweis University Professor Csaba Bödör who is the Head of the Department of Molecular Diagnostics at Semmelweis University’s Institute of Pathology and Experimental Cancer Research. According to him, the basic question of the examination is whether the patient carries a gene variant, a disease-related molecular deviation, for which some known drug is already available.
“Like in pediatric oncology, the main goal in the case of adult patients is to identify new therapeutic targets, which is currently possible by a next-generation sequencing examination focusing on more than 500 genes, performed with a new-generation sequencer (Illumina, Trusight Oncology 500). The NEAK committee, which meets weekly, decides on the state financing of this at the initiative of the attending physicians,” said Semmelweis University Professor Csaba Bödör who is the Head of the Department of Molecular Diagnostics at Semmelweis University’s Institute of Pathology and Experimental Cancer Research. According to him, the basic question of the examination is whether the patient carries a gene variant, a disease-related molecular deviation, for which some known drug is already available.
At Semmelweis University, this pediatric oncogenomics initiative was launched in 2019, which later grew to be a nationwide profiling program operated jointly with the Pediatric Oncology Network. Thanks to this, 25 percent of the patients examined so far were able to receive individualized, targeted therapy. Subsequently, a pilot program was launched at the institution in November 2020, in the framework of which more than 400 comprehensive genomic profiling of 500 genes were completed by the end of 2021 regarding several types of adult tumors.
With the introduction of state funding for oncogenomic profiling, patients’ chances have improved further since January 2022,
and a structured and searchable database built from the results of the tests is constantly expanding, which can help researchers to identify gene variants and gene fusions that can be used as new therapeutic targets.
 Since January 2022, the National Molecular Oncoteam has received a total of 544 cases nation-wide, in the case of 78 percent of which the 500-gene test was approved. Only 3 percent of children and a third of adults were refused the examination for various reasons. Looking at it based on tumor type, 100 percent of brain, 91 percent of hematological, and 92 percent of soft tissue tumor patients were supported with NEAK-funded testing. The National Molecular Oncoteam also provided funding for comprehensive profiling in 75 percent of gynecological, 56 percent of pancreatic, 49 percent of colorectal, 33 percent of gallbladder tumors, and 26 percent of breast cancer cases.
Since January 2022, the National Molecular Oncoteam has received a total of 544 cases nation-wide, in the case of 78 percent of which the 500-gene test was approved. Only 3 percent of children and a third of adults were refused the examination for various reasons. Looking at it based on tumor type, 100 percent of brain, 91 percent of hematological, and 92 percent of soft tissue tumor patients were supported with NEAK-funded testing. The National Molecular Oncoteam also provided funding for comprehensive profiling in 75 percent of gynecological, 56 percent of pancreatic, 49 percent of colorectal, 33 percent of gallbladder tumors, and 26 percent of breast cancer cases.
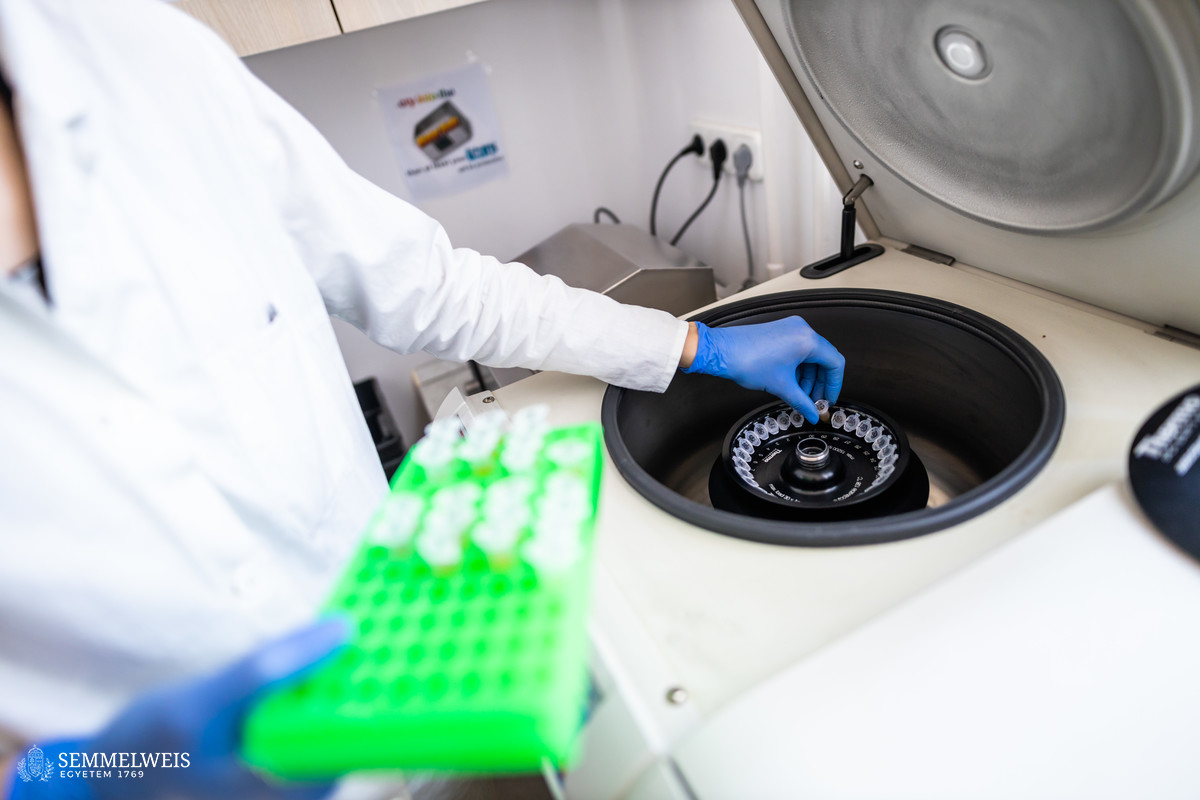
During the procedure related to comprehensive genetic profiling, at the request of the attending physician and after the approval of NEAK, the oncology centers send the patient’s tissue sample to the university, where nucleic acid is isolated from it, and DNA and RNA are analyzed using next-generation sequencing, determining the most important genetic differences. The findings of the comprehensive genomic profiling are usually completed in 3-4 weeks and are followed by a consultation with the clinicians. As a result of the profiling, so-called prognostic and predictive biomarkers are identified, which help the physician to assess how molecular differences affect the treatment strategy, whether the patient can receive targeted therapy, and, if so, what kind exactly.
At the same time, in a smaller proportion of cases, a deviation can be detected that can help patients with targeted therapy, said Dr. Csaba Bödör. The specialist added that there are also tumor types, such as colon tumors or non-small cell lung cancer, in which instead of the 500-gene NGS test, the panels typically testing 50-200 genes on outpatient bases can also lead to adequate results and they do not require an official permit from NEAK.
A workshop on the latest scientific and procedural information related to molecular diagnostic tests was held on May 24 for nearly a hundred interested oncologists at Semmelweis University.
Melinda Katalin Kiss
Translation: Mária Sánta
Photos: Bálint Barta, Attila Kovács — Semmelweis University