The ‘Curriculum 2.0. – Workshop’ was opened by the rector of Semmelweis University. According to Dr. Béla Merkely, the goal is not only to preserve the institution’s more than 250-year-old traditions and knowledge left by predecessors, but also to proactively contribute to this knowledge, becoming more and better every day.
We were the first to reform the curriculum of medical education at national level, and today we can say that all six of our faculties have undergone some level of training revision: either as a result of the already introduced Curriculum 1.0, or as a result of re-accreditation, or precisely because, in response to new and changing needs, the faculties themselves were continuously developing their education
– the rector said.
 He then pointed out that in recent years, a paradigm shift has been observed in higher education, with the emphasis shifting from knowledge transfer to results-based training. The aim of this is to guarantee that upon receiving their diploma, graduating students already possess the skills and knowledge that enable them to competently perform the tasks that await them. “We must also take this into account when revising the curriculum. To sum it up, a university must constantly reflect on its own courses, the satisfaction of students, clinical and labor market stakeholders, as well as our University’s international recognition. By revising and developing our curriculum, we have to ensure that the quality of education here is competitive at the international level,” he stressed.
He then pointed out that in recent years, a paradigm shift has been observed in higher education, with the emphasis shifting from knowledge transfer to results-based training. The aim of this is to guarantee that upon receiving their diploma, graduating students already possess the skills and knowledge that enable them to competently perform the tasks that await them. “We must also take this into account when revising the curriculum. To sum it up, a university must constantly reflect on its own courses, the satisfaction of students, clinical and labor market stakeholders, as well as our University’s international recognition. By revising and developing our curriculum, we have to ensure that the quality of education here is competitive at the international level,” he stressed.
The workshop’s keynote speech was delivered by Dr. György Purebl, the Director of the Institute of Behavioral Sciences at the Faculty of Medicine, about the trends and changing needs in higher education. He started out saying that the frequency of mental disorders is increasing in all ages, and unfortunately, medical students are not exempt either. Generally speaking, there is a discrepancy between ambitions and possibilities, which results in frustration, anxiety, and depression. “This is topped with the burden of traditional methodology aspects like an excessive amount of lexical information, subject competition instead of subject integration, difficult and unpredictable exams, so an overload during most of the process. As a result, according to international surveys, every third student experiences emotional exhaustion and burnout right after graduation,” he explained.
 As for possible solutions, Dr. György Purebl outlined a series of suggestions. Along with a comprehensive semester plan, curriculum and learning materials should be revised, parallel teaching and ’prestige contests’ should be avoided, exams are supposed to be more predictable, and students should be more involved in general. “Skills training and active mentoring should increase. We are expected to educate expertise, not just facts,” the director said. According to Dr. György Purebl, a novel set of teacher’s skills are needed, which includes digital proficiency, the ability to motivate, mentor and support the actual learning process, recognition and first response to emotional difficulties and distress, and last but not least, pedagogical methodology skills.
As for possible solutions, Dr. György Purebl outlined a series of suggestions. Along with a comprehensive semester plan, curriculum and learning materials should be revised, parallel teaching and ’prestige contests’ should be avoided, exams are supposed to be more predictable, and students should be more involved in general. “Skills training and active mentoring should increase. We are expected to educate expertise, not just facts,” the director said. According to Dr. György Purebl, a novel set of teacher’s skills are needed, which includes digital proficiency, the ability to motivate, mentor and support the actual learning process, recognition and first response to emotional difficulties and distress, and last but not least, pedagogical methodology skills.
The workshop continued with presentations from the Theoretical and Preclinical Training Working Group and the Working Group for Clinical Training, both delegated by the Faculty of Medicine, followed by the Working Groups of the Faculties of Dentistry, of Pharmaceutical Sciences, of Health Sciences, the András Pető Faculty and the Faculty of Health and Public Administration. In the framework of the presentations, the working groups reported on the six-month process and methodology of the training revision and experiences thereof, including the strengths and challenges of the trainings, as well as a summary overview of the tasks identified, and the action plans formulated along these lines.
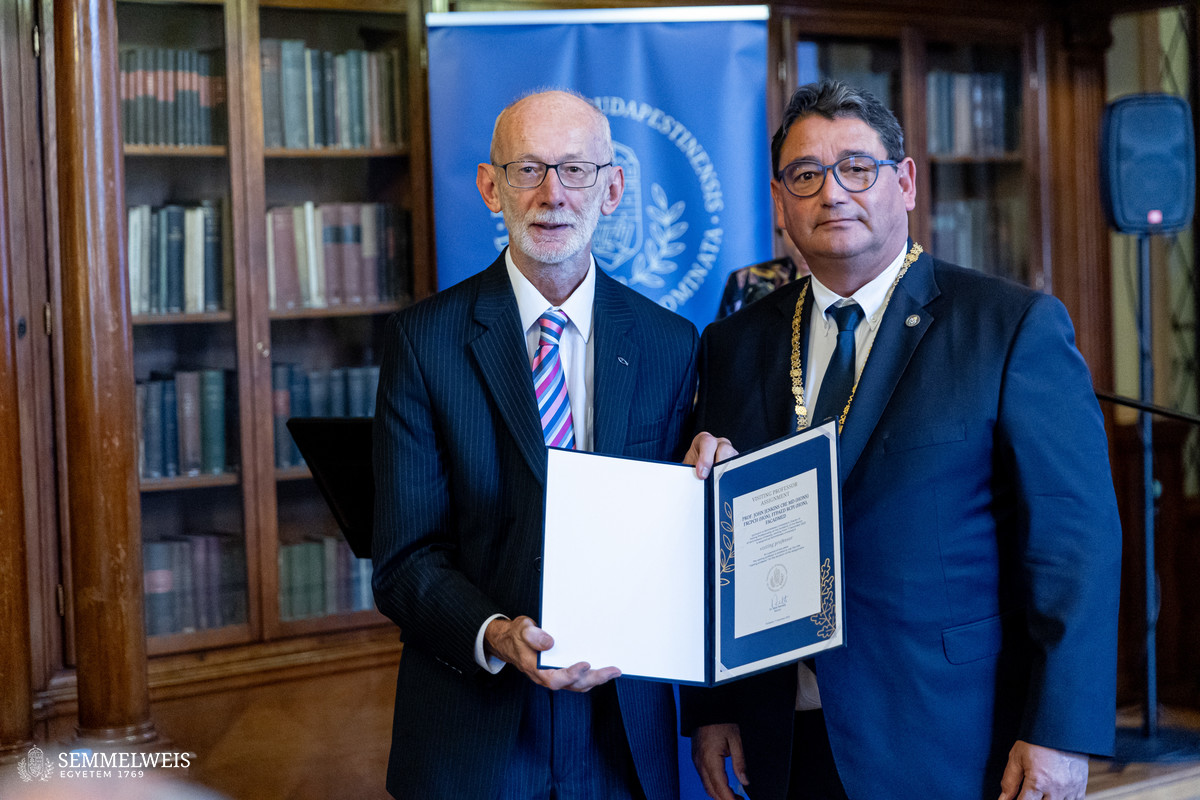
John Jenkins, Honorary Professor at the RCSI University of Medicine and Health Sciences, Ireland, and Chair of the ASPIRE Award Board of the International Association for Health Professions Education (AMEE), opened the row of invited expert speakers to talk about the role of the award in curriculum development. The ASPIRE Award is presented in nine areas, including curriculum development, but, as the speaker pointed out, the underlying aim of the program is to contribute to improving the quality of medical and health education by collecting and sharing the best practices from the winning entries and providing a platform for an exchange of experiences. In outlining the criteria for an effective curriculum, he stressed that its review should take into account external factors such as demographic trends or the emergence of new scientific disciplines, in addition to feedback from graduates, current students and clinicians, and should reflect national settings as well as responses to international labor market mobility needs.
 In an ideal curriculum, knowledge is not assembled as pieces of a puzzle, but rather integrated as connected cogwheels, said Dr. John Jenkins. He believes that a spirally structured curriculum is highly effective, which revisits a topic as the training progresses, but increasingly synthesizes it. For example, the pediatrics module initially focuses on lactation and weaning, which is later complemented by the biochemistry of neonatal metabolism. The success of a training course is also facilitated by assigning students to sub-tasks for which they already possess the necessary knowledge as early as possible in the clinical training. As Dr. John Jenkins emphasized, the training review also aims to raise awareness that the body of knowledge in medicine has long exceeded the cognitive capacity of a single individual, shifting the focus to teaching learning and the timing of when interprofessional collaboration becomes necessary.
In an ideal curriculum, knowledge is not assembled as pieces of a puzzle, but rather integrated as connected cogwheels, said Dr. John Jenkins. He believes that a spirally structured curriculum is highly effective, which revisits a topic as the training progresses, but increasingly synthesizes it. For example, the pediatrics module initially focuses on lactation and weaning, which is later complemented by the biochemistry of neonatal metabolism. The success of a training course is also facilitated by assigning students to sub-tasks for which they already possess the necessary knowledge as early as possible in the clinical training. As Dr. John Jenkins emphasized, the training review also aims to raise awareness that the body of knowledge in medicine has long exceeded the cognitive capacity of a single individual, shifting the focus to teaching learning and the timing of when interprofessional collaboration becomes necessary.
 Tim Dornan, Emeritus Professor at Maastricht University and Queen’s University Belfast, gave a lecture on the philosophical background to medical education. As he explained, the learning sciences seek to answer the questions of what, why and how. The Hippocratic Oath of the 5th century BC included not only questions of medical ethics, but also components related to medical education and the transmission of knowledge, such as respect for teachers and imparting knowledge to those who took the oath. According to the idea attributed to the ancient Greek physician, medicine is a practice (in answer to the question of ‘what?’) that serves the benefit of society (‘why?’) by balancing the benefits with the potential risks (‘how?’). The Flexner Report, which laid the foundations for the present-day American medical profession, supplemented this with the requirement of scientific evidence. After theories such as self-directed or problem-based learning, which reflected the current zeitgeist, many medical education programs have now reached the point where teaching is limited to knowledge that can be reliably trained and tested (‘what?’), assessed by measurable tests (‘how?’), and designed to satisfy compliance with regulations (‘why?’). As a way forward, he identified practice- and student-centered education, a collaboration between students, teachers, and patients, in which students can quickly put into practice the repetitive skills they had previously drilled, while at the same time extracting the most useful knowledge from ‘teachable moments’ encountered in clinical practice.
Tim Dornan, Emeritus Professor at Maastricht University and Queen’s University Belfast, gave a lecture on the philosophical background to medical education. As he explained, the learning sciences seek to answer the questions of what, why and how. The Hippocratic Oath of the 5th century BC included not only questions of medical ethics, but also components related to medical education and the transmission of knowledge, such as respect for teachers and imparting knowledge to those who took the oath. According to the idea attributed to the ancient Greek physician, medicine is a practice (in answer to the question of ‘what?’) that serves the benefit of society (‘why?’) by balancing the benefits with the potential risks (‘how?’). The Flexner Report, which laid the foundations for the present-day American medical profession, supplemented this with the requirement of scientific evidence. After theories such as self-directed or problem-based learning, which reflected the current zeitgeist, many medical education programs have now reached the point where teaching is limited to knowledge that can be reliably trained and tested (‘what?’), assessed by measurable tests (‘how?’), and designed to satisfy compliance with regulations (‘why?’). As a way forward, he identified practice- and student-centered education, a collaboration between students, teachers, and patients, in which students can quickly put into practice the repetitive skills they had previously drilled, while at the same time extracting the most useful knowledge from ‘teachable moments’ encountered in clinical practice.
 Dr. Krisztina Fischer, Faculty Director at Harvard Medical School (HMS), presented the curriculum reforms implemented at the institution. Although all reforms have a philosophical or theoretical basis, at the end of the day, they are about people: firstly, alleviating patient suffering; secondly, the student community; thirdly, faculty development; and finally, staff. Curriculum3 reform is imperative, as the rapid development of medicine and health science means that half of the knowledge taught today will be wrong or irrelevant by the time current students retire, and it is therefore the task of education to prepare our students for lifelong learning.
Dr. Krisztina Fischer, Faculty Director at Harvard Medical School (HMS), presented the curriculum reforms implemented at the institution. Although all reforms have a philosophical or theoretical basis, at the end of the day, they are about people: firstly, alleviating patient suffering; secondly, the student community; thirdly, faculty development; and finally, staff. Curriculum3 reform is imperative, as the rapid development of medicine and health science means that half of the knowledge taught today will be wrong or irrelevant by the time current students retire, and it is therefore the task of education to prepare our students for lifelong learning.
HMS believes that the continuous development of medicine and its underlying educational technology, along with the instant access to information, allow for the so-called ‘flipped classroom’ model, said Dr. Krisztina Fischer. Under this method, students learn the concepts at home, which they give an account of by taking a short readiness test. The aim of the class is to apply the theoretical knowledge to clinical cases, working in teams to solve problems. The method was refined in the pilot phase in light of students’ study time and mental workload, so that student feedback actively contributed to the successful course design and a balanced workload. The practice-oriented approach is reflected in the structure of the curriculum, combining theoretical and clinical education on a weekly basis, allowing the goal of healing to remain in focus despite the assessments. Furthermore, basic theoretical training is followed by clinical practice, and this experience is used as a basis for continuing the training with advanced theoretical subjects. Referring back to the philosophy of education, Dr. Krisztina Fischer pointed out:
Education is not only about imparting knowledge, but also about shaping the student and providing an inspiring learning environment. This is not only a societal issue, but also a personal one: today’s educators must teach their students as if they were training their own doctors, as today’s students will be at the peak of their careers when their teachers will be in need of clinical care
– Dr. Krisztina Fischer concluded.
As the closing ceremony of the workshop, Dr. Béla Merkely, Rector of Semmelweis University, presented certificates of two-year visiting professorial appointments to Professors John Jenkins, Tim Dornan and Krisztina Fischer.
Viktória Kiss, Judit Szabados-Dőtsch
Photo: Attila Kovács – Semmelweis University