Investigation of the possible association between lithium levels in drinking water and suicide mortality in Hungary
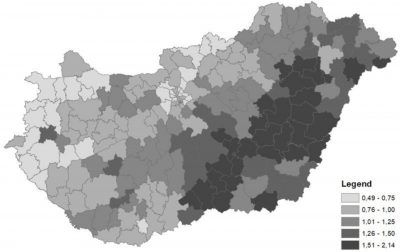
Lithium (Li) has been part of the therapeutic armamentarium of psychiatry for decades, mainly used in the treatment of severe mood disorders, i.e. bipolar disorder and major depression. There is strong evidence that lithium, in addition to reducing the symptoms of mood disorders, provides a strong protective effect against suicidal behaviour in these patients. Li is also present in drinking water as a trace element, but typically in such low concentrations that we would need to consume tens of thousands of litres of tap water a day to consume the dose established for medical use. Nevertheless, a number of studies in different countries have shown that even the minimum amount of Li in drinking water can reduce the risk of suicide in the average population.
“In our study, we were the first to demonstrate that this effect can also be detected in our country (the study was conducted on aggregated data at the district level). According to the results, the suicide prevention effect of Li is mainly seen among males, which is probably due to the fact that they frequently choose more violent methods to commit suicides than females, and the anti-aggressive and anti-impulsive effect of Li is mainly able to prevent these deaths,” Dr. Péter Döme said in his summary.
Investigation of the association between lithium levels in drinking water and suicide mortality in Hungary
Balint Izsak (National Public Health Center; Eotvos Lorand University, Doctoral School of Environmental Sciences), Anna Hidvegi (Department of Internal Medicine I, Military Hospital, Hungarian Defense Forces Medical Center), Lajos Balint (Demographic Research Institute of the Hungarian Central Statistical Office; Department of Sociology, University of Pécs), Tibor Malnasi (National Public Health Center), Marta Vargha (National Public Health Center), Tamas Pandics (National Public Health Center), Zoltan Rihmer (Department of Psychiatry and Psychotherapy, Semmelweis University; Nyiro Gyula National Institute of Psychiatry and Addictions), Peter Dome (Department of Psychiatry and Psychotherapy, Semmelweis University; Nyiro Gyula National Institute of Psychiatry and Addictions)
Journal of Affective Disorders, Vol. 298, Part A, pp. 540-547, 2022
https://doi.org/10.1016/j.jad.2021.11.041
Acute Pain Service in Hungarian hospitals
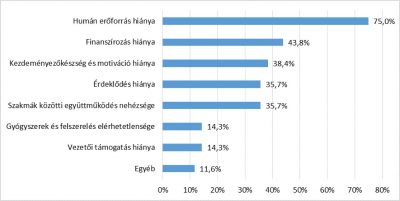
Pain after surgical interventions is a significant burden for both the patient and the healthcare system. After surgery, some patients experience moderate to severe pain, which can limit their ability to carry out daily activities and can cause anxiety, fear and depression, hindering the healing process. Multidisciplinary Acute Pain Services (APS) are a new form of care in hospitals that help to reduce the patient’s pain and treatment-related side-effects, improve patient safety and patient satisfaction. The research examined the availability and characteristics of APS in Hungary, their educational and quality activities and the barriers to their development.
“At present, only two hospitals have postoperative pain management teams, one made up of doctors and the other of healthcare professionals supervised by an anaesthetist. Their operations are in line with the literature. The need to set up these services is also recognized in hospitals that don’t have an APS. Lack of staff and funding were mentioned as the main obstacles to their establishment, but lack of motivation and initiative, and difficulties in cooperation between surgical specialties were also mentioned as important problems,” Dr Orsolya Lovasi wrote in her summary.
Acute Pain Service in Hungarian hospitals
Orsolya Lovasi (School of PhD Studies, Semmelweis University), Judit Lam (Semmelweis University Health Services Management Training Centre), Reka Schutzmann (School of PhD Studies, Semmelweis University), Peter Gaal (Semmelweis University Health Services Management Training Centre)
PLoS ONE 16(9)
https://doi.org/10.1371/journal.pone.0257585
CAD-RADS may underestimate coronary plaque progression as detected by serial CT angiography
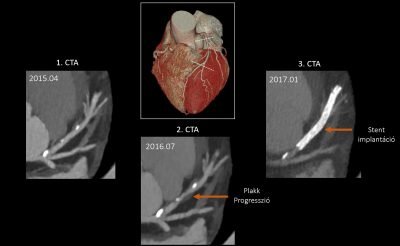
Coronary artery disease (CAD) is a chronic disease with dynamic temporal changes in plaque size and composition. Coronary computed tomography angiography (CTA) is a robust, non-invasive diagnostic test to characterize CAD. Coronary plaque progression is an independent predictor of cardiovascular events, but its definition is not uniform. Our aim was to determine plaque progression according to the different definitions currently used for the severity and extent of coronary artery disease. We also analysed which risk factors influence the progression of CAD. We enrolled 115 subsequent patients who underwent serial coronary computed tomography angiography at the Városmajor Heart and Vascular Center of Semmelweis University.
“Our results showed significantly different levels of progression using different definitions. It should be highlighted that the so-called CAD-RADS (coronary artery disease – reporting and data system) classification used in the clinic did not identify plaque progression in more than half of the cases, in contrast to other definitions. In addition, diabetes, smoking, male gender and age influenced the progression of coronary plaques significantly,” Dr. Borbála Vattay and Dr. Bálint Szilveszter summarized.
CAD-RADS may underestimate coronary plaque progression as detected by serial CT angiography
Balint Szilveszter (MTA-SE Cardiovascular Imaging Research Group, Heart and Vascular Center, Semmelweis University), Borbala Vattay (MTA-SE Cardiovascular Imaging Research Group, Heart and Vascular Center, Semmelweis University), Melinda Bossoussou (MTA-SE Cardiovascular Imaging Research Group, Heart and Vascular Center, Semmelweis University), Milan Vecsey-Nagy (MTA-SE Cardiovascular Imaging Research Group, Heart and Vascular Center, Semmelweis University), Judit Simon (MTA-SE Cardiovascular Imaging Research Group, Heart and Vascular Center, Semmelweis University), Béla Merkely (MTA-SE Cardiovascular Imaging Research Group, Heart and Vascular Center, Semmelweis University), Pál Maurovich-Horvat (MTA-SE Cardiovascular Imaging Research Group, Heart and Vascular Center, Semmelweis University; Medical Imaging Centre, Semmelweis University), Márton Kolossváry (MTA-SE Cardiovascular Imaging Research Group, Heart and Vascular Center, Semmelweis University)
European Heart Journal – Cardiovascular Imaging, jeab215, 2021
https://doi.org/10.1093/ehjci/jeab215
Association of Body Mass Index with clinical outcomes in patients with cystic fibrosis
The study investigates the link between body mass index (BMI) and various clinical outcomes in patients with cystic fibrosis. Over the past two decades, life expectancy in this disease has increased significantly (currently 47 years in the US), giving way to phenomena that were not previously considered, such as obesity.
“The results suggest that a higher than normal BMI resulted better lung function (FEV1%) and more favourable exocrine and endocrine status in pancreatic function. The highly complex meta-analysis points to the need to replace the current nutritional recommendations (22 kg/m2 and 23 kg/m2) with a higher target BMI for patients with CF. Based on these results, a new therapeutic strategy is needed in the nutrition of patients, which could bring them significant health benefits,” Dr Andrea Párniczky and Dr Rita Nagy summarised.
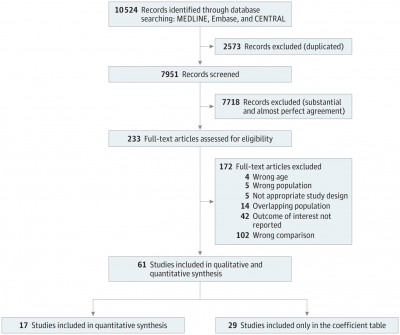
Association of Body Mass Index With Clinical Outcomes in Patients With Cystic Fibrosis. A Systematic Review and Meta-analysis
Rita Nagy (Institute for Translational Medicine, Szentágothai Research Centre, Medical School, University of Pécs; Centre for Translational Medicine, Semmelweis University; Heim Pál National Pediatric Institute), Noemi Gede (Institute for Translational Medicine, Szentágothai Research Centre, Medical School, University of Pécs), Klementina Ocskay (Institute for Translational Medicine, Szentágothai Research Centre, Medical School, University of Pécs), Bernadett-Miriam Dobai (Institute for Translational Medicine, Szentágothai Research Centre, Medical School, University of Pécs; George Emil Palade University of Medicine, Pharmacy, Science and Technology of Targu Mures), Alan Abada (Institute for Translational Medicine, Szentágothai Research Centre, Medical School, University of Pécs; Department of Anaesthesiology and Intensive Therapy, Medical School, University of Pécs), Zsofia Vereczkei (Institute for Translational Medicine, Szentágothai Research Centre, Medical School, University of Pécs), Piroska Pazmany (Institute for Translational Medicine, Szentágothai Research Centre, Medical School, University of Pécs; Heim Pál National Pediatric Institute; Doctoral School of Clinical Medicine, University of Szeged), Dorottya Kato (Institute for Translational Medicine, Szentágothai Research Centre, Medical School, University of Pécs), Peter Hegyi (Institute for Translational Medicine, Szentágothai Research Centre, Medical School, University of Pécs; Centre for Translational Medicine, Semmelweis University; Division of Pancreatic Diseases, Heart and Vascular Center, Semmelweis University), Andrea Parniczky (Institute for Translational Medicine, Szentágothai Research Centre, Medical School, University of Pécs; Centre for Translational Medicine, Semmelweis University; Heim Pál National Pediatric Institute)
JAMA Netw Open, 5(3):e220740, 2022
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2789687
Further scientific publications:
The short summaries were made by the authors of the scientific publications.
Edited by Ádám Szabó, translation by Rita Kónya
Photo illustrations: images from the publications