HIPEC treatment stands for ‘hyperthermic intraperitoneal chemotherapy’, which is used in combination with extended abdominal surgery. The method, introduced for the treatment of ovarian cancer, is used by specialists in certain cases of appendix and colon cancer and is also effective in some other oncological diseases. In his welcome address at the ceremony marking the 100th HIPEC procedure, Dr. Szabolcs Máté, Head Physician of the Gynecological Oncology and Tumor Surgery Unit of the Department of Obstetrics and Gynecology, said that the purpose of the gathering was not only to celebrate this new milestone, but also to bring together all those who participated in the program, both on the medical side and as patients. “We tried to put together the presentations in such a way as to show how multifaceted this procedure is and how many people’s coordinated work is required to perform it,” Dr. Szabolcs Máté pointed out.
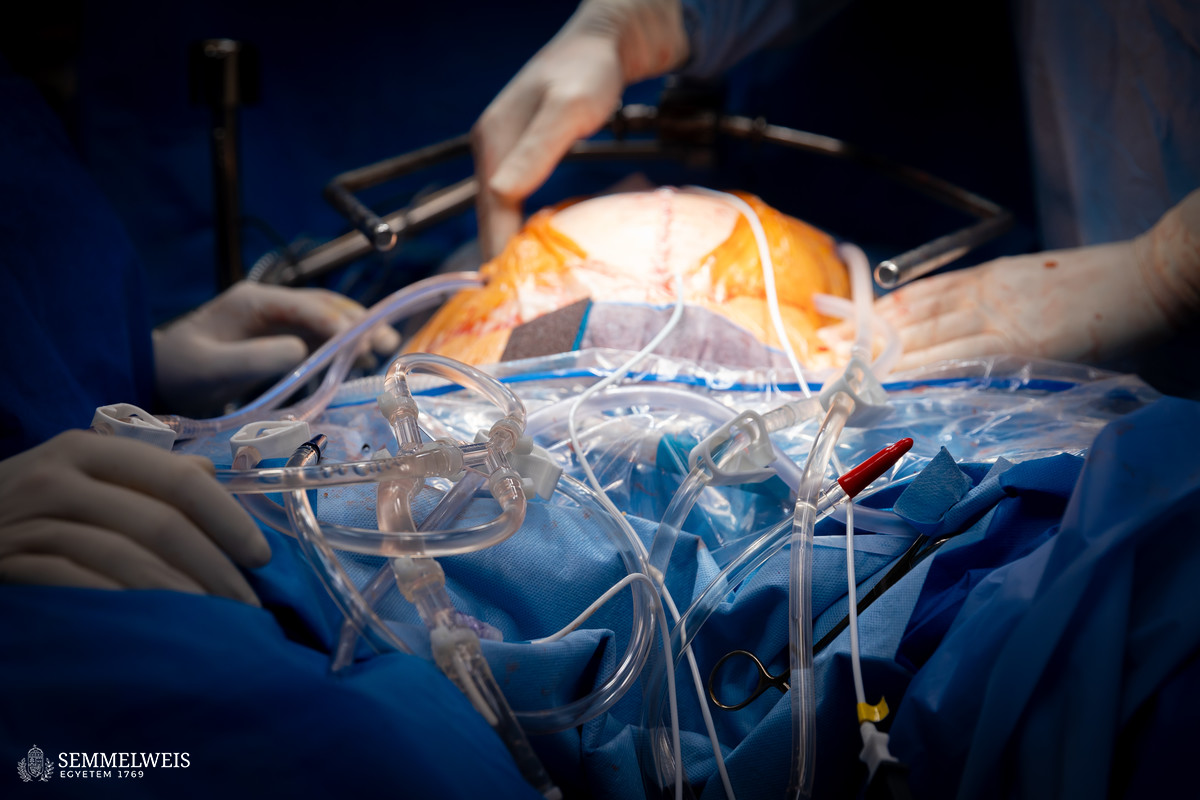
The first presentation at the event was given by Dr. Gergely Huszty, Assistant Professor at the Department of Surgery, Transplantation and Gastroenterology (STéG), who spoke about the technical and professional background of the surgeries. One of the things he explained was that the working group – from among the various procedures used worldwide – had chosen the method in which, after the complete removal of the tumor or tumors, the sutured abdominal cavity is further treated with chemotherapy. Another important part of the protocol is that in the case of very extensive tumors, at least two senior surgeons are present in the operating room to take turns during long and exhausting surgeries, if necessary.
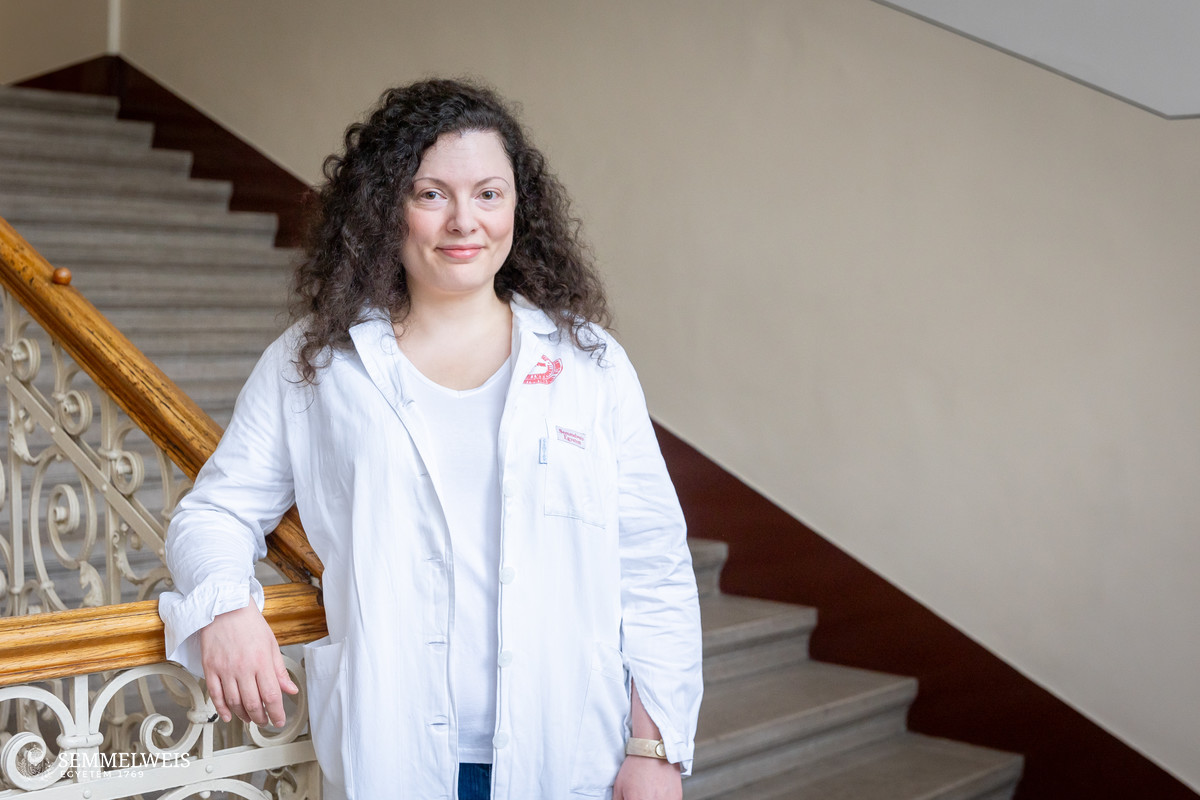
Dr. Márkó Unicsovics, a Clinical Specialist at the Department of Obstetrics and Gynecology, discussed the chemotherapy part of HIPEC treatment, pointing out that, according to studies, the department’s protocol of bathing the abdominal cavity with heated chemotherapy drugs was more effective in terms of patient recovery and, with appropriate protective clothing, chemotherapy drugs had no measurable effect on healthcare personnel.
Ovarian cancer is not classified as one of the most common tumorous diseases, yet around 1,300 new cases are diagnosed and almost 700 women die from it every year in Hungary, as Dr. Sándor Nyíri, Assistant Lecturer at the Department of Obstetrics and Gynecology, noted in his presentation. The biggest challenge is that nearly 60 percent of cases are diagnosed at an advanced stage, when survival rates are already poor. During surgery, complete tumor removal must be achieved. The basic idea behind HIPEC treatment is that heating can enhance the cell-killing effect of chemotherapy and that a much higher concentration of the chemotherapy solution can be achieved when it is delivered directly into the abdominal cavity. The survival data from the studies presented show that members of the patient group who received HIPEC live an average of 12 months longer than those who did not receive such treatment.
In his second presentation, Dr. Gergely Huszty discussed the effectiveness of the HIPEC procedure in the treatment of other tumors associated with peritoneal dissemination. He underlined that the Semmelweis University working group was unique in that, in addition to surgeons, a gynecological oncologist was also present during these operations. The method is currently used mainly for tumors of the appendix and colon cancer, with good results.
After that, Dr. Orsolya Gerlai, specialist at the Institute of Anesthesiology and Perioperative Patient Care, spoke about the importance of proper surgical preparation and anesthesiologic tasks during surgeries which often last 6-8 hours. Dr. Zsuzsanna Marjanek, Head Physician at the Intensive Therapy Clinic, then presented the postoperative tasks and considerations.
Dr. Szabolcs Máté summarized the departmental history of HIPEC treatments to date. As he pointed out, parallel to the introduction of the procedure, several devices had been purchased for the department in the areas of patient monitoring, electrosurgery, surgical smoke evacuation, ultrasound equipment, and lighting, and further similar developments were planned within the framework of the program. Among the results, he mentioned that the Baross Street and Üllői Street sections of the Department of Obstetrics and Gynecology had been jointly accredited by the European Society of Gynaecological Oncology (ESGO) as an ovarian cancer surgery center. He also shared a number of interesting facts with the attendees, for instance that the longest surgery to date had been 570 minutes long, and that HIPEC procedures lasted an average of 300 minutes. In most cases, patients can be discharged one week after surgery. He emphasized the role of the entire team, thanking not only the doctors, anesthesiologists, and nurses, but also the perioperative nurses, physiotherapists, psychologists, dieticians, and administrative staff for their work. Among their future plans, Dr. Szabolcs Máté mentioned the publication of the results and the improvement of surgical preparation.
Eszter Keresztes
Translation: Dr. Balázs Csizmadia
Photos by Boglárka Zellei – Semmelweis University