The Hematopathology Mini Symposium was hosted by the Department of Pathology and Experimental Cancer Research, whose Head, Dr. András Matolcsy, briefly welcomed the speakers. This was followed by a welcome address by Rector Dr. Béla Merkely. In his speech, the rector recalled that the focus of the event, hematopathology, had come into being through ever new discoveries and become a separate discipline within pathology.
Although the discipline is relatively young, its roots date back over a century. Nobel Prize-winning German scientist Paul Ehrlich, who was one of the first to study blood cells and their staining properties, was born ten years after Lajos Arányi delivered his inaugural lecture in Hungary in 1844, thus paving the way for pathology as a discipline in its own right. – Dr. Béla Merkely
 The rector pointed out that Times Higher Education’s latest ranking put Semmelweis among the top 300 universities in the world. The same ranking lists the University of Chicago, where Dr. Daniel A. Arber is the Chair of Pathology, in the 14th position. That is why I consider his presentation today extremely important and a great opportunity to learn from the best, he added. The event was attended by the leaders and members of the Hungarian Society of Pathologists and the Hungarian Society of Haematology and Transfusion (MHTT), heads of department from Semmelweis University, and experts in molecular oncohematology research from Hungarian partner universities. Dr. Béla Merkely said that this was a great pleasure for him, as the university’s goal was to put international exchange in the service of domestic healthcare and the interest of patients in Hungary.
The rector pointed out that Times Higher Education’s latest ranking put Semmelweis among the top 300 universities in the world. The same ranking lists the University of Chicago, where Dr. Daniel A. Arber is the Chair of Pathology, in the 14th position. That is why I consider his presentation today extremely important and a great opportunity to learn from the best, he added. The event was attended by the leaders and members of the Hungarian Society of Pathologists and the Hungarian Society of Haematology and Transfusion (MHTT), heads of department from Semmelweis University, and experts in molecular oncohematology research from Hungarian partner universities. Dr. Béla Merkely said that this was a great pleasure for him, as the university’s goal was to put international exchange in the service of domestic healthcare and the interest of patients in Hungary.
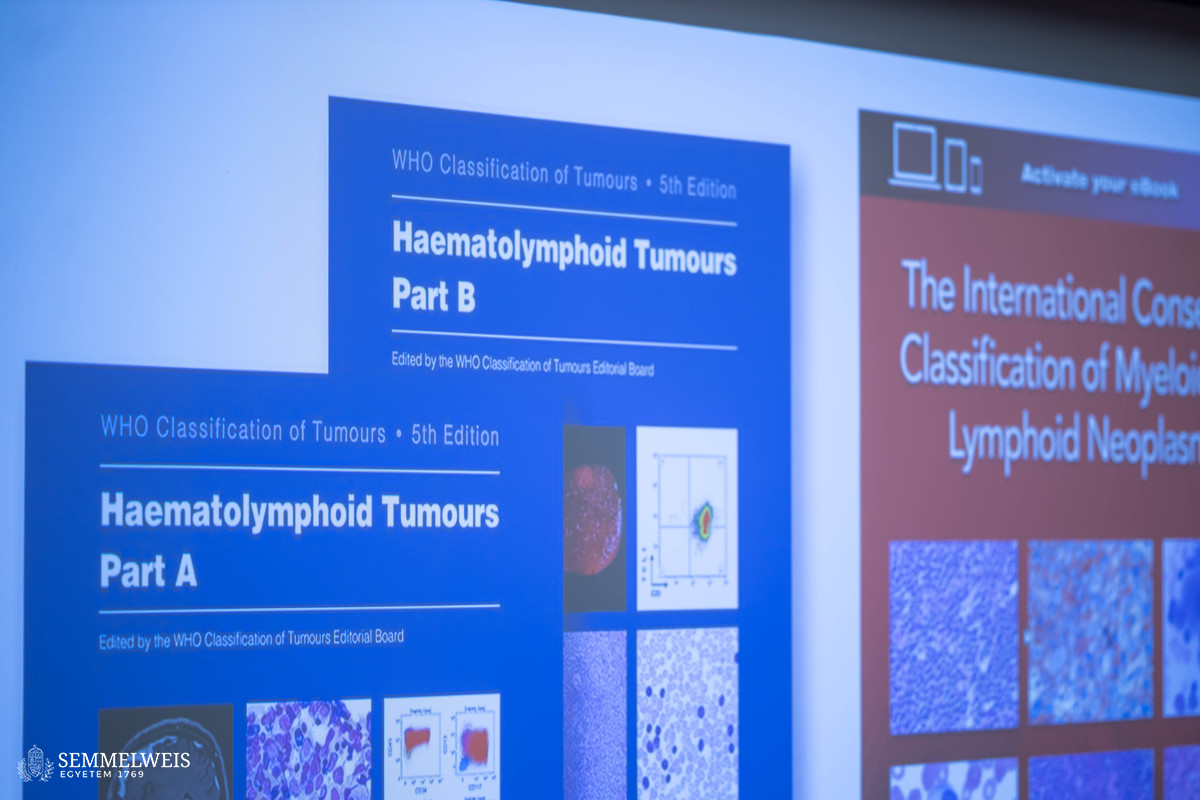
A central element of modern diagnostics, risk assessment, and therapeutic planning in the case of hematological tumors is the increasingly precise classification of diseases on a molecular basis. Dr. Daniel A. Arber is an internationally renowned authority in this field and has pioneered the development of the classification of acute myeloid leukemia (AML), one of the most serious types of blood cancer. His talk first explored how our understanding of myeloid neoplasms – and AML in particular – had evolved from early, imprecise observations to sophisticated, genetics-based classification systems. He traced the history of myeloid neoplasms from the 1800s, when leukemia was studied without microscopes, through major breakthroughs in pathology to the introduction of systematic classifications. Dr. Daniel A. Arber pointed out that modern classification systems, such as those of the World Health Organization (WHO) and the International Consensus Classification (ICC) for the categorization of myeloid and lymphoid neoplasms, increasingly incorporate genetic data to make the correct diagnosis and design appropriate treatment. Although both systems are now used, there is more than 90 percent overlap between them, a sign of increasing scientific precision and reliability. Dr. Daniel A. Arber is a lead editor on The International Consensus Classification of Myeloid and Lymphoid Neoplasms, a volume that focuses on diagnostic criteria and the clinical significance of each disease entity.
 The professor and chair of the Department of Pathology at the University of Chicago went on to investigate how genetic mutations shape the classification and treatment of AML. The way these mutations interact can dramatically impact prognosis and guide treatment. Researchers no longer rely primarily on cell appearance (i.e. dysplasia, the presence of abnormal cells within a tissue or organ) to make a diagnosis but instead classify AML on the basis of genetic mutations, which are considered to be more accurate indicators. As a result of this change, some classification categories have become simpler, while others more complicated, particularly for mutations in the TP53 gene associated with malignant tumors. Among experts, there is a growing awareness of therapy-related and inherited forms of AML, which is now clearly reflected in diagnoses. While current classification systems differ only slightly, a unified global standard is being prepared for 2026, which aims to make AML diagnosis even faster, more precise, and globally consistent.
The professor and chair of the Department of Pathology at the University of Chicago went on to investigate how genetic mutations shape the classification and treatment of AML. The way these mutations interact can dramatically impact prognosis and guide treatment. Researchers no longer rely primarily on cell appearance (i.e. dysplasia, the presence of abnormal cells within a tissue or organ) to make a diagnosis but instead classify AML on the basis of genetic mutations, which are considered to be more accurate indicators. As a result of this change, some classification categories have become simpler, while others more complicated, particularly for mutations in the TP53 gene associated with malignant tumors. Among experts, there is a growing awareness of therapy-related and inherited forms of AML, which is now clearly reflected in diagnoses. While current classification systems differ only slightly, a unified global standard is being prepared for 2026, which aims to make AML diagnosis even faster, more precise, and globally consistent.
 Dr. Csaba Bödör, Professor at the Department of Pathology and Experimental Cancer Research, said that the department was playing an increasingly important role at the national level in advanced diagnostics for blood cancers such as leukemia and lymphoma. His research team is working with hospitals across Hungary to study both children and adults, using powerful genetic tools such as next-generation sequencing (NGS) and optical genome mapping. These tools help doctors to detect hidden mutations and better understand individual cancers. In children, this has led to the discovery of new genetic markers and better prediction of disease progression. In adults, the research team is investigating whether the new technologies can outperform older genetic tests. They are also studying rare inherited mutations that run in families, helping to select the right treatment and donor. In addition to leukemia, the team is also working to improve the diagnosis of lymphoma using both tissue and blood samples, with the aim of predicting relapses in patients early. Dr. Csaba Bödör stressed that collaboration and innovation are key to personalized medicine.
Dr. Csaba Bödör, Professor at the Department of Pathology and Experimental Cancer Research, said that the department was playing an increasingly important role at the national level in advanced diagnostics for blood cancers such as leukemia and lymphoma. His research team is working with hospitals across Hungary to study both children and adults, using powerful genetic tools such as next-generation sequencing (NGS) and optical genome mapping. These tools help doctors to detect hidden mutations and better understand individual cancers. In children, this has led to the discovery of new genetic markers and better prediction of disease progression. In adults, the research team is investigating whether the new technologies can outperform older genetic tests. They are also studying rare inherited mutations that run in families, helping to select the right treatment and donor. In addition to leukemia, the team is also working to improve the diagnosis of lymphoma using both tissue and blood samples, with the aim of predicting relapses in patients early. Dr. Csaba Bödör stressed that collaboration and innovation are key to personalized medicine.
The Department of Pathology and Experimental Cancer Research, which is more than 180 years old, provides diagnostic services for acute leukemias to several clinical hematology centers in the country, and the Department of Internal Medicine and Hematology is involved in the treatment of a large number of patients with acute leukemia. Under the leadership of Dr. András Matolcsy, the national diagnostic center for hematopathology has been operating for more than 20 years. Over the past five years, modern molecular oncohematology research and diagnostic instrument infrastructure has been developed, which enables the department to diagnose patients with acute leukemia to the highest international standards. It also provides support for patients and their doctors in other hematology centers around the country.
Dr. Balázs Csizmadia
Photos by Bálint Barta – Semmelweis University