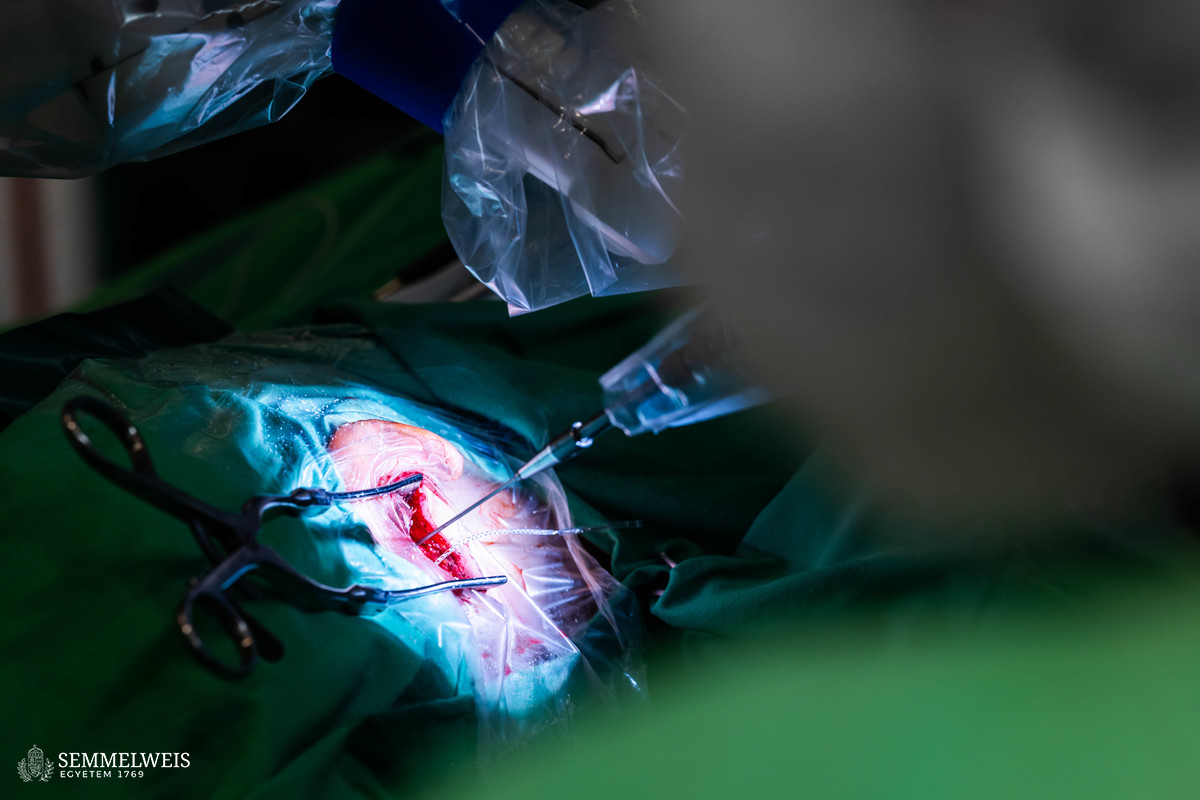
“At the beginning of March, we successfully restored the hearing of four patients by using an ear surgery robot to insert the vital part of the cochlear implant into the cochlea of the patients’ inner ear,” Dr. László Tamás, Director of the Department of Otorhinolaryngology, Head and Neck Surgery, told our website. He explained that among the head and neck surgeries performed at the department, hearing correction procedures – including the insertion of so-called cochlear implants – played a prominent role. The procedure involves implanting a highly sophisticated, special computer into the patient’s skull through a 3-4-centimeter incision behind the auricle and inserting an extremely thin electrode, about 0.3 millimeters in diameter at the end, into the patient’s inner ear, with which their hearing can be restored under the right conditions. The procedure can be used to treat children born with hearing loss due to genetic causes, infectious diseases contracted during pregnancy, or other problems, as well as patients who have lost their hearing due to various forms of trauma, illness, injury, or age-related sensory impairment.
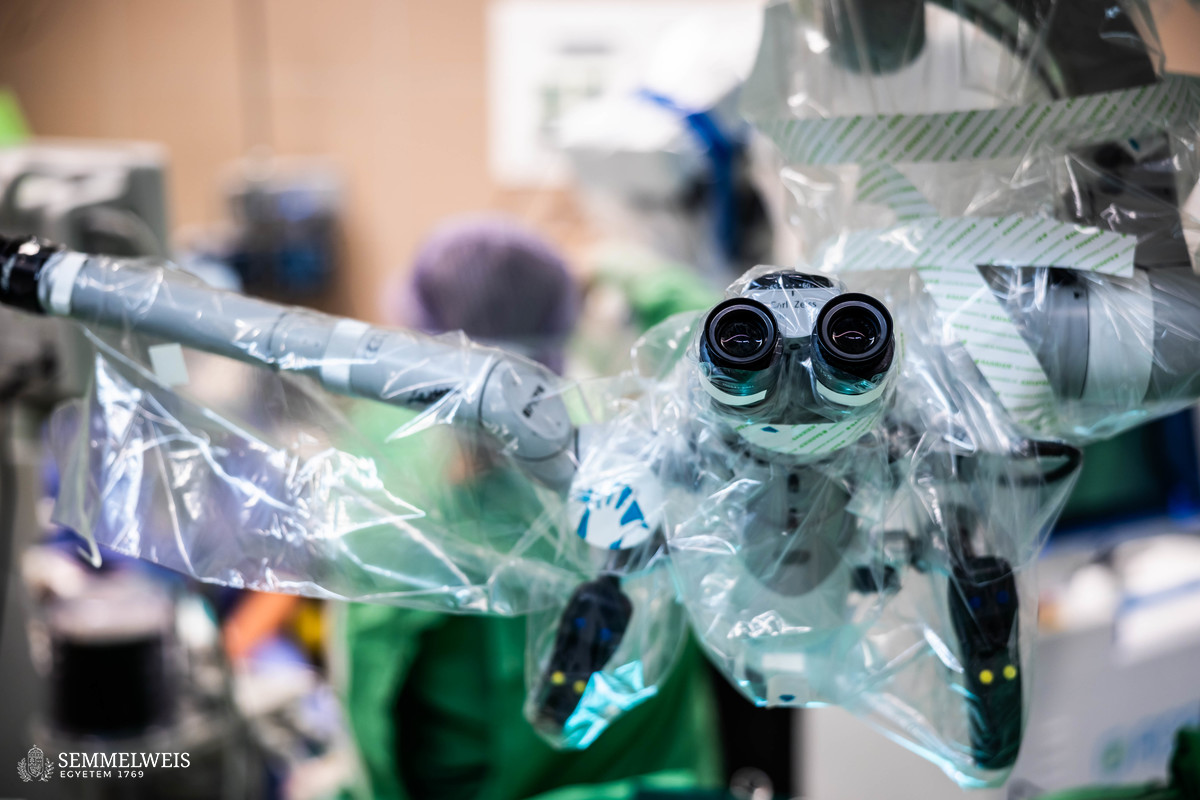
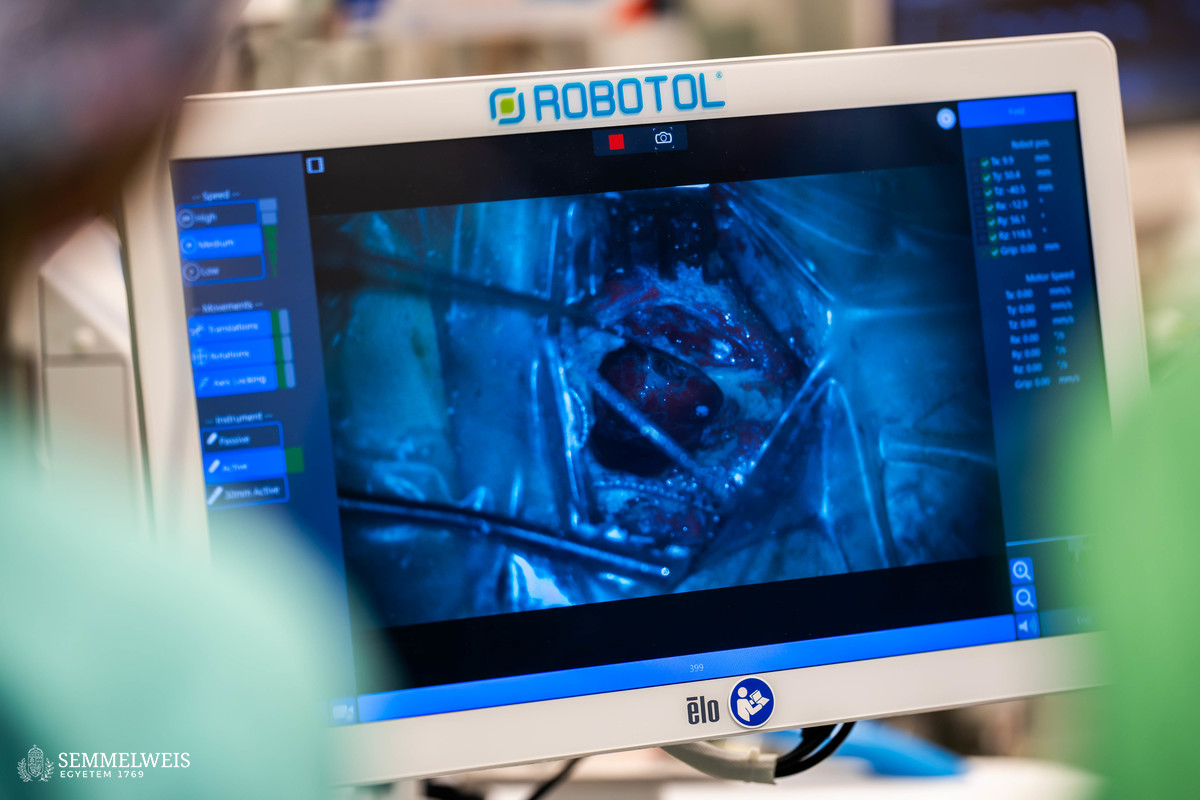
 “The surgical procedure for the robot is the same as when surgeons use a microscope to perform the implantation. The RobOtol ear surgery robot we have just tested helps surgeons to insert the electrode into the inner ear very slowly, evenly, and precisely, so that the structure of the inner ear and the hair cells that may still be left can be better preserved,” said Dr. Gábor Polony, Associate Professor at the department, the surgeon who was in charge of the operations, and who had learned how to use the robot in a training course abroad. In special cases, the implant can also serve as a hearing aid in the still-functioning part of the cochlea, and as a cochlear implant where the hair cells have died. “With the use of the currently available surgical robots, knowledge of anatomy and ear surgery for these procedures remains essential for the person carrying out the operation,” stressed Dr. Gábor Polony, who added that in the near future the department would be able to test another ear surgery robot that had come onto the market in recent years, and they also hoped to be involved in the development of devices.
“The surgical procedure for the robot is the same as when surgeons use a microscope to perform the implantation. The RobOtol ear surgery robot we have just tested helps surgeons to insert the electrode into the inner ear very slowly, evenly, and precisely, so that the structure of the inner ear and the hair cells that may still be left can be better preserved,” said Dr. Gábor Polony, Associate Professor at the department, the surgeon who was in charge of the operations, and who had learned how to use the robot in a training course abroad. In special cases, the implant can also serve as a hearing aid in the still-functioning part of the cochlea, and as a cochlear implant where the hair cells have died. “With the use of the currently available surgical robots, knowledge of anatomy and ear surgery for these procedures remains essential for the person carrying out the operation,” stressed Dr. Gábor Polony, who added that in the near future the department would be able to test another ear surgery robot that had come onto the market in recent years, and they also hoped to be involved in the development of devices.
The robot-assisted surgeries just performed have been successful, and all patients will hopefully be able to hear. – Dr. László Tamás
The specialists base this assessment of the situation partly on the results of telemetry measurements of the neural response during surgery (to check the response of the auditory nerve during the operation) and partly on CT scans taken after the implant was inserted. Following the successful interventions, all patients were discharged within two days, and rehabilitation following implantation will begin soon. In the complex audiological and rehabilitation program developed at the department, hearing and speech training as well as speech development are supported – alongside specialists and engineers – by a special education teacher, an audiologist, and a psychologist.
The implant itself is made up of two parts: a receiver unit implanted into the skull behind the auricle, with a 12, 16, or 22-channel electrode at the end, which is inserted into the cochlea in the inner ear, replacing the dead (or non-formed) hair cells of the cochlea to deliver electrical signals to the endings of the auditory nerve; and the outer unit containing the directional microphone, which is connected to the implanted unit through the intact skin by a magnet and converts the detected sounds into electrical signals, transmitting them to the inner unit. The outer unit of implants has also undergone enormous development in recent decades.
One of the great successes of the profession is the mandatory screening of newborn babies’ hearing in hospitals since 2015, which allows early detection of hearing problems in babies. Between three and five per thousand babies born on term are hard of hearing or have hearing loss, but the rate is much higher for premature babies (between one and three percent).
Because the cochlea of the inner ear is formed by newborn age and does not grow any further, the ideal time for implantation is between one and two years of age. By this time, it will be clear whether the child is hard of hearing or has a complete congenital hearing loss. – Dr. László Tamás
Early implantation allows for effective speech learning with proper rehabilitation, and by the age of about three, the child’s speech understanding and speech production will be established. “Advances in technology, diagnostics, and surgical procedures have made it possible to perform the intervention as early as one year of age,” Dr. László Tamás added. The intervention should be performed at the latest by the age of five to six. For adults, we aim to perform the implantation as soon as possible, even within one to two months after an injury or an inflammation that causes hearing loss, Dr. Gábor Polony said.
 At present, we perform unilateral or bilateral hearing implants on roughly the same number of young children as adults to improve their hearing. This currently means 50-60 procedures per year at the department, Dr. László Tamás noted. He also recalled that it was thanks to the former director of the department, Dr. Ottó Ribári, that the first cochlear implantations were performed in Hungary in 1985 – in fact, they were the first among the socialist countries of that time and the third in Europe to do so.
At present, we perform unilateral or bilateral hearing implants on roughly the same number of young children as adults to improve their hearing. This currently means 50-60 procedures per year at the department, Dr. László Tamás noted. He also recalled that it was thanks to the former director of the department, Dr. Ottó Ribári, that the first cochlear implantations were performed in Hungary in 1985 – in fact, they were the first among the socialist countries of that time and the third in Europe to do so.
The Department of Otorhinolaryngology, Head and Neck Surgery has also held middle ear surgery cadaver training courses for Hungarian specialists in recent years under the leadership of Dr. Gábor Polony, which have attracted considerable interest. “In the medium term, we would like to develop this into an international course, for which we already have the internal professional experience and international contacts,” added Dr. László Tamás, speaking about the future of the department.
Melinda Katalin Kiss
Translation: Dr. Balázs Csizmadia
Photos by Bálint Barta – Semmelweis University