The recent explosion in the use of genetics, molecular biology, cell biology, informatics, data science, artificial intelligence, nanotechnology, and laboratory technology, as well as the increase in international research have accelerated the study of stem cell therapy to find cures for certain diseases.
Most professionals predict that the next stem cell therapy will be available for safe clinical use within 10-15 years. – Dr. Nándor Nagy
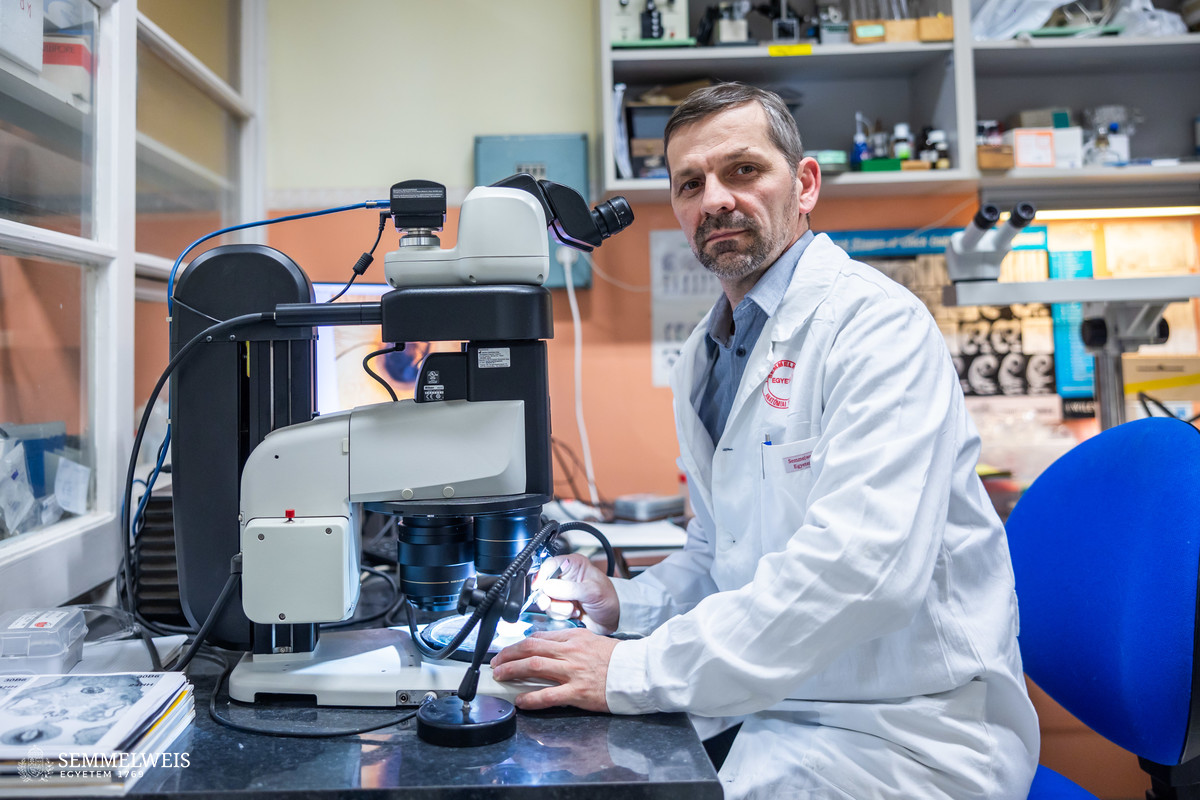
According to Professor Dr. Nándor Nagy – Deputy Director for Science at the Department of Anatomy, Histology and Embryology; Coordinator of the Embryology, Theoretical, Experimental and Clinical Developmental Biology PhD program; and Head of the Laboratory of Stem Cell and Experimental Embryology -, when he took over the leadership of the basic research laboratory back in 2007, stem cell research focused on understanding how stem cells develop into tissues and cells, how stem cells can be isolated and propagated, and whether reliable transplantation techniques can be developed. Subsequently, the clinical need for medical application emerged, which gave rise to applied stem cell research. This aims to offer safe stem cell therapies for other diseases, available as soon as possible, even in the medium term, to enable the introduction of treatments at least as effective and successful as bone marrow transplantation for leukemia, various lymphomas, and anemia. Stem cell transplantation has been available in Hungary since the 1980s, in four hospital centers. In the summer of 2024, Semmelweis University also introduced the intervention, which is financed by the National Health Insurance Fund of Hungary (NEAK).
Nowadays, science is mainly focused on the safe application of stem cell therapy to ensure that the stem cells, whether transplanted from the patient’s own cells or donor cells, achieve the desired therapeutic effect without the risk of abnormal cell proliferation, i.e. tumor formation, and as cost-effectively as possible. Once this becomes biologically safe, it will pave the way for the routine use of stem cell therapy and regenerative medicine, predicts Dr. Nándor Nagy. For the time being, existing stem cell therapies mostly involve transplanting back the patient’s own stem cells, while bone marrow transplants involve weakening the patient’s immune system with drugs to make it accept donor cells. Although there are several cell banks in Europe and about 7,000 registered donors in Hungary, the transplantation of stem cells programmed and propagated under laboratory conditions from donor blood stem cells is not yet in clinical use.
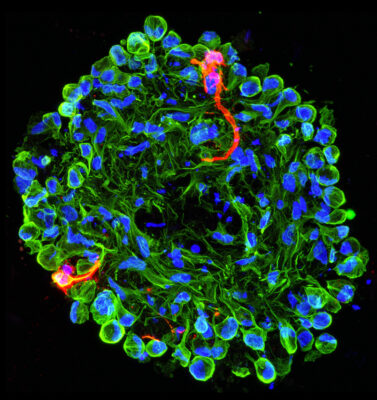
In practice, regenerative medicine is concerned with the development of therapies to replace or restore organs that are damaged, degenerating, or malfunctioning due to developmental disorders or infections, and stem cells can be used to create transplantable cells or miniature organs, so-called organoids, for diseases that cannot be treated with drugs, explains Dr. Nándor Nagy. The transplantation of organoids is also a promising line of research, as many believe that the transplantation of artificially created miniature organs – for example, pancreatic organoids instead of insulin-producing cells – is a guarantee that the transplant will only work for the purpose intended by the therapy.
 The laboratory led by Dr. Nándor Nagy focuses on stem cell-based therapeutic options for the development of the intestinal tract and the enteric nervous system and for the treatment of neurointestinal diseases, including Hirschsprung’s disease, causing congenital colon enlargement. Patients with this condition have no bowel movement, and the contents of the colon are not passed through the colon, causing the affected section of the intestine to become inflamed and the intestinal wall to die. Currently, this can only be treated by surgical removal of the damaged section of the colon showing necrosis – a life-saving procedure often required in infancy; there is no cure, and the condition requires regular medical monitoring.
The laboratory led by Dr. Nándor Nagy focuses on stem cell-based therapeutic options for the development of the intestinal tract and the enteric nervous system and for the treatment of neurointestinal diseases, including Hirschsprung’s disease, causing congenital colon enlargement. Patients with this condition have no bowel movement, and the contents of the colon are not passed through the colon, causing the affected section of the intestine to become inflamed and the intestinal wall to die. Currently, this can only be treated by surgical removal of the damaged section of the colon showing necrosis – a life-saving procedure often required in infancy; there is no cure, and the condition requires regular medical monitoring.
Our basic research to understand the biological basis of the developmental biology of the enteric nervous system has shown that it is not enough to develop and transplant a stem cell in the desired direction, it must also be aligned with the host tissue to prevent rejection or abnormal cell proliferation. We have been researching this for the last five years, but we are also paying special attention to the role of the immune system. – Dr. Nándor Nagy
“We are striving to develop a stem cell transplantation technique to correct developmental defects in the colon and to establish the scientific basis for this. We are the only research group in Hungary and Central and Eastern Europe working on stem cell therapy for Hirschsprung’s disease, and we have close research collaborations with French, English, and Israeli researchers as well as with a group of American doctors,” the head of the laboratory points out.
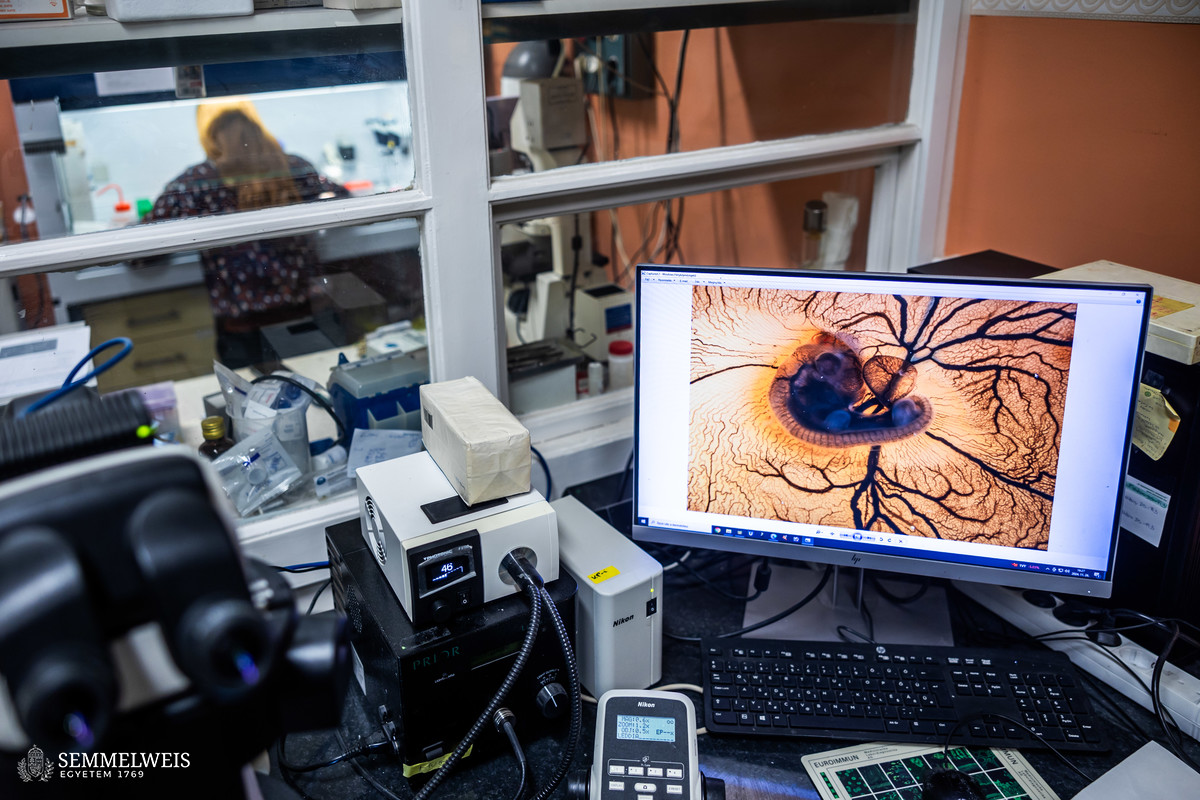
In recent years, the collaboration has succeeded in murine studies as well as in transplanting stem cells from the small intestine of porcine models back into the colon after differentiating them into neural stem cells, thus proving the validity of the laboratory-developed method.
In the longer term, the aim is to find a cure for neurological disorders by reprogramming induced pluripotent stem cells and then transplanting them into human tissue and developing them into neural cells. The lab is currently studying the behavior of human-derived programmed stem cells in embryonic settings using murine and avian embryos. The results of this basic research will soon be applied in a preclinical phase by a US research team using damaged intestinal segments removed from patients diagnosed with Hirschsprung’s disease.
As stem cell therapies enter the human experimental phase, their number will also increase worldwide if the laboratory costs of human stem cell propagation can be significantly reduced, i.e. if bioreactors can be developed and disseminated for the production and cultivation of large numbers of stem cells with sufficient purity. Due to its significant laboratory requirements which make it the most expensive treatment option, even today, stem cell therapy is only considered when an organ has been irreversibly damaged and stopped. However, the scientific community is unanimous that within 10 years more diseases will be safely curable with stem cell therapies, Dr. Nándor Nagy emphasizes. The deputy director expects that once these therapies become more widespread in the clinical setting, the education of medical embryology and developmental biology, as well as theoretical and applied stem cell therapy will also be given greater emphasis in medical training.
Melinda Katalin Kiss
Translation: Judit Szabados-Dőtsch
Photos by Bálint Barta – Semmelweis University