In addition to reducing cardiovascular diseases, one of the key strategic objectives of Hungary’s EU Council presidency, which started on July 1, is to further increase the number of transplants following the decline in organ transplantation across Europe during the COVID pandemic. The low point in national data was 2020-2021, after which a gradual increase started.
 “In 2023, we have already performed 20 more liver transplants than in 2020, with a total of 70 such procedures, an increase of 40 percent. There has also been a significant increase in kidney transplants at Semmelweis University over the past three years, with an increase of almost 30 percent,” said Dr. Attila Szijártó, Director of the Department of Surgery, Transplantation and Gastroenterology (STéG). In terms of kidney transplants, the decline caused by the COVID pandemic was mitigated by the timely initiation and reconsideration of the live-donor kidney transplantation program; in 2022, we performed 40 live-donor transplants, the highest number of live-donor donations and transplants compared to previous decades, Dr. Attila Szijártó emphasized.
“In 2023, we have already performed 20 more liver transplants than in 2020, with a total of 70 such procedures, an increase of 40 percent. There has also been a significant increase in kidney transplants at Semmelweis University over the past three years, with an increase of almost 30 percent,” said Dr. Attila Szijártó, Director of the Department of Surgery, Transplantation and Gastroenterology (STéG). In terms of kidney transplants, the decline caused by the COVID pandemic was mitigated by the timely initiation and reconsideration of the live-donor kidney transplantation program; in 2022, we performed 40 live-donor transplants, the highest number of live-donor donations and transplants compared to previous decades, Dr. Attila Szijártó emphasized.
Liver transplantation is performed only here in the whole country, and its centralized form ensures the quality indicators achieved in transplantation that in many respects far exceed the European average, the director stressed.
Liver, kidney, and pancreas transplantation – as part of a comprehensive professional unit
Kidney transplantation is available at all four university centers in the country, but the department at Semmelweis University is the largest center; in 2023, a total of 265 kidney transplants were performed in Hungary, with more transplants carried out at STéG (148 in total, more than half of the activity at a national level) than at the three other centers altogether. 11 combined kidney and pancreas transplantations were performed nationally, 9 of which at the department at Semmelweis University.
As Dr. Attila Szijártó noted:
Analyzing the figures for the first half of this year, we believe there is a good chance that we can return to or even exceed pre-pandemic levels in both kidney and liver transplants.
The director emphasized that this September would mark three years since abdominal organ (liver, kidney, pancreas) transplantation at Semmelweis University became part of a comprehensive professional unit, the Department of Surgery, Transplantation and Gastroenterology (STéG). “In terms of the results we have achieved and the data, our organ transplantation activities continue to be of international standard, and in some respects even ahead of some major European centers,” said Director Dr. Attila Szijártó, summing up the results achieved since the establishment of the new organizational structure.
In recent years, the department has seen a number of developments and innovations aimed at increasing the number of successful transplants and transplant activity.
At the end of last year, the first split liver transplantation was performed in Hungary, which saved two lives by splitting a donor organ. This was followed by another successful split transplant in 2024, so we are proud to say that we have saved the lives of two children and two young adults with the split livers from two donors, the director pointed out.
Semmelweis University is the largest transplant center in Hungary, and its role is unquestionable at a regional level as well. It was the first to launch organized transplantation programs at the national level: For example, the first kidney transplantation to ensure long-term survival (1973) and the first liver transplantation (1983) were performed here, a complex liver transplantation program (1995) was launched, and the first heart transplantation (1992) was carried out. The first lung transplantation in Hungary (2005) was performed in cooperation between Semmelweis University and the National Institute of Oncology.
In order to ensure adequate transplant activity, it is essential that all patients whose lives could be saved with this intervention are put on the waiting list. As the leading center for hepatology and liver surgery in the country, STéG pays special attention to increasing the number of cancer patients on the liver waiting list. One of the most recent achievements of the department is the development of a protocol for the treatment of liver tumors that are the result of metastasis (e.g. colon cancer metastasis) by transplantation (RAPID protocol). “This is a much more complex procedure than the one we use for primary liver cell cancer as only live-donor transplantation is possible, which needs to be performed in two rounds by gradually implanting the new liver segments and removing the parts affected by the tumor,” the director noted.
For patients requiring kidney transplantation, a new electronic patient referral system (Fyrms) has been implemented to support the waiting list process, replacing paper-based history-taking and follow-up, and to maintain continuous contact with dialysis centers. This is a breakthrough for more accurate and efficient patient selection, which is essential in the hours before transplantation, the director said.
Managing to perform a higher number of live-donor transplants is an important means of increasing the number of transplants in general, which can benefit greatly from providing patients as well as family members and relations with information. Visits by members of the department to kidney dialysis centers and the production of a short film served this purpose.
3D design and modelling are now part of the preparation for live-donor kidney transplants, which make it possible to plan in advance how the organ will be positioned in the patient. This is another important milestone in terms of patient safety and surgical efficiency, Dr. Attila Szijártó stressed.
The department has also completed the professional preparation of “ABO-incompatible transplants,” a procedure that – after acceptance by NEAK (the National Health Insurance Fund of Hungary) – allows for kidney transplants to be performed between donors and recipients of different blood types.
According to Dr. Attila Szijártó, in the next six months it may be possible to use the da Vinci surgical system to remove a kidney from a living donor in a robot-assisted operation, which will allow for an even more precise procedure with even less stress for the donor.
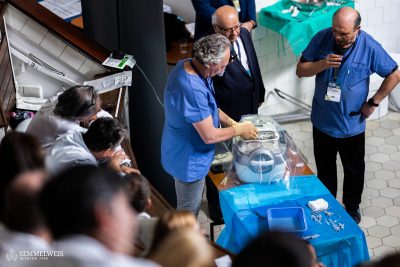
Special emphasis was also placed on the professional development of organ procurement; in this context, a “donor surgery masterclass” was held.
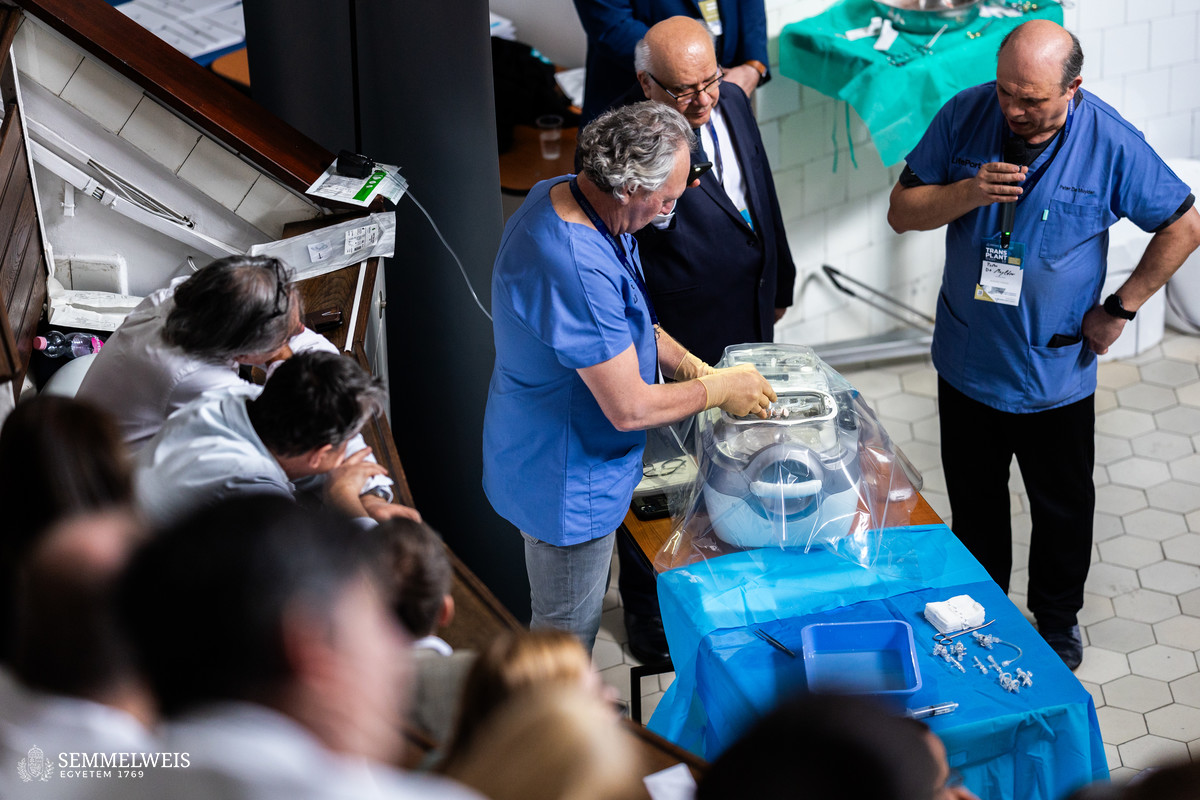
Machine perfusion is an important means of further increasing the number of organs available for transplantation, which was the topic of this year’s Transplant Today, the department’s third training event of this kind. While the introduction of machine perfusion is a national issue, the department is planning to purchase and use such a device in clinical trials, and a faculty member has been on a study tour to Padua to explore the subject.
Aftercare of transplant patients is a priority for the department. It provides aftercare for nearly 3,200 kidney transplant and 1,400 liver transplant patients, involving 14,000-15,000 doctor-patient meetings per year for the former and 6,300 for the latter. These figures have remained unchanged for years, the number of specialists has not decreased, and, in fact, it has even increased by one hepatologist and two nephrologists; altogether, three hepatologists, eight nephrologists, as well as four resident doctors are involved in this type of care.
A 44-bed matrix-like ward provides treatment, pre- and post-transplant care for transplant patients, and a new, modern transplant intensive care unit meeting all professional requirements is being built.
Dr. Attila Szijártó also pointed out that Hungary had been a member of Eurotransplant, the largest organ allocation organization at European level which brings together 8 member states, for 11 years now. This represents a huge opportunity to increase the number of organs available for transplantation, as on average 25 percent of all organs transplanted today reach Hungarian patients through Eurotransplant. Dr. Attila Szijártó also believes that the results and experiences of this collaboration so far could serve as a model for a broader, common EU strategy.
Lung transplantation: the result of exemplary European cooperation
“There are only a few countries in the Central and Eastern European region with a well-functioning lung transplant program, one of which is Hungary, where the quality of the interventions is at the forefront of European standards,” emphasized Dr. Ferenc Rényi-Vámos, Director of Semmelweis University’s Department of Thoracic Surgery based at the National Institute of Oncology.
 As he pointed out, the Hungarian program was the result of truly exemplary European cooperation. The first lung transplantation in Hungary took place in 2015, in cooperation between Semmelweis University and the National Institute of Oncology (OOI), and it was performed jointly by Dr. Ferenc Rényi-Vámos and Dr. György Lang. Prior to this, lung transplantation for Hungarian patients had been performed in Vienna, where the Hungarian team had also prepared for the first procedure. “After the first three years, the Hungarian program became fully self-sufficient, and now we are able to receive patients from other Eastern European countries, for example from Serbia or Macedonia – as long as we have the capacity to do so besides caring for Hungarian patients, of course,” Dr. Ferenc Rényi-Vámos noted.
As he pointed out, the Hungarian program was the result of truly exemplary European cooperation. The first lung transplantation in Hungary took place in 2015, in cooperation between Semmelweis University and the National Institute of Oncology (OOI), and it was performed jointly by Dr. Ferenc Rényi-Vámos and Dr. György Lang. Prior to this, lung transplantation for Hungarian patients had been performed in Vienna, where the Hungarian team had also prepared for the first procedure. “After the first three years, the Hungarian program became fully self-sufficient, and now we are able to receive patients from other Eastern European countries, for example from Serbia or Macedonia – as long as we have the capacity to do so besides caring for Hungarian patients, of course,” Dr. Ferenc Rényi-Vámos noted.
In the past nearly 10 years, an average of 20 lung transplants have been performed annually, but the COVID pandemic – as it has done everywhere else in the world – has hit this area very hard since it put an additional burden especially on pulmonologists and intensive care units. At the same time, specialists in Hungary were able to use the experience gained with ECMO (extracorporeal membrane oxygenation) during lung transplantation very well for the care of the most severe COVID patients requiring artificial lung treatment.
According to Dr. Ferenc Rényi-Vámos, after the end of the pandemic, even if slowly, an increase in the numbers could be felt based on the data of the first half of this year; but in the case of lung transplantation, the real breakthrough would be if even more lung patients were added to the waiting list – to this end, he himself is visiting Hungarian lung care centers to disseminate the necessary information.
“With the launch of the Hungarian lung transplant program, we have brought cutting-edge technology and a cutting-edge procedure to Hungary,” the director said. He added that the next step in the development of the technology could be the use of the da Vinci robot in the field of lung transplant surgery, but this is still in the experimental phase at an international level as well. However, in principle, the means to do it are already available in Hungary, since in addition to Semmelweis University, the OOI – at the base of which lung transplants take place – also has a robotic surgical system in place, which is already used routinely for almost all thoracic surgery.
In the field of heart transplantation, Semmelweis University’s Városmajor Heart and Vascular Center is among the top 10 heart transplant centers in the world, according to ISHLT (International Society for Heart and Lung Transplantation) data. Semmelweis University has moved up in the U.S. News 2024-2025 Best Global Universities Rankings to 31st position in cardiac and cardiovascular systems. Click here to read our article on the rankings.
Pálma Dobozi
Translation: Dr. Balázs Csizmadia
Photos by Attila Kovács, Bálint Barta – Semmelweis University