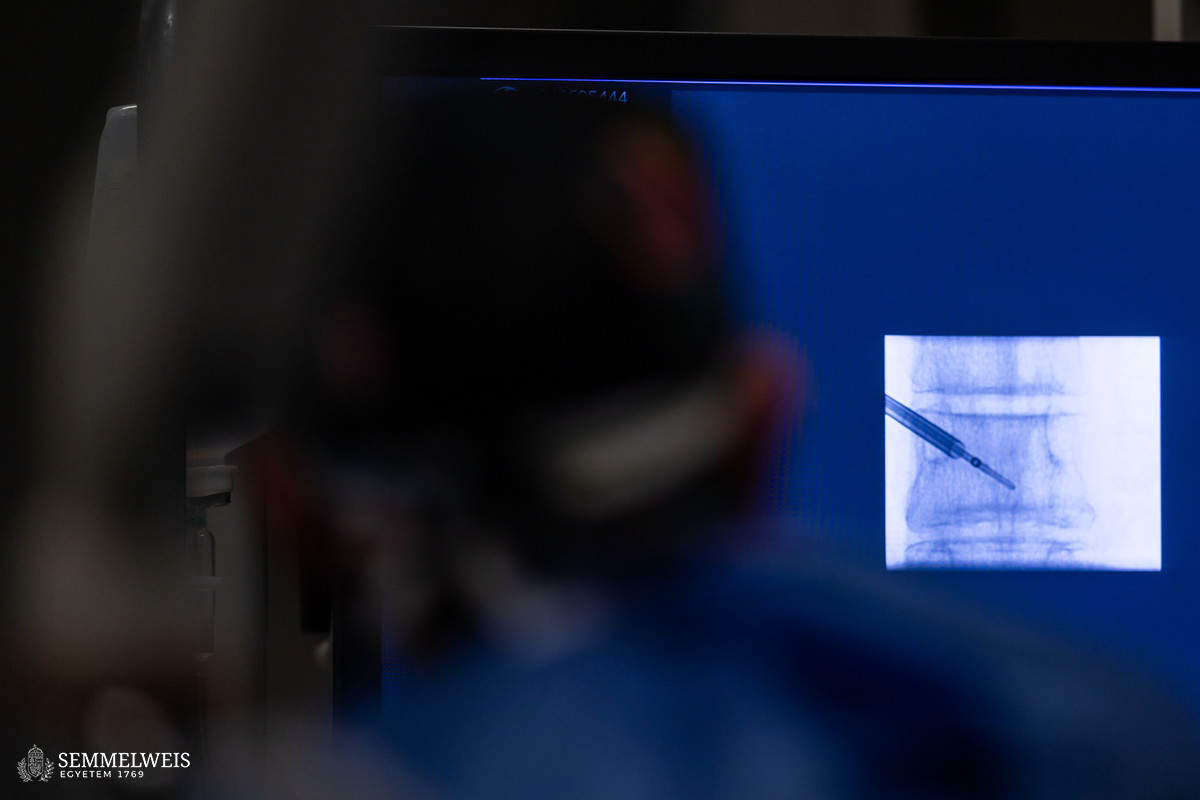
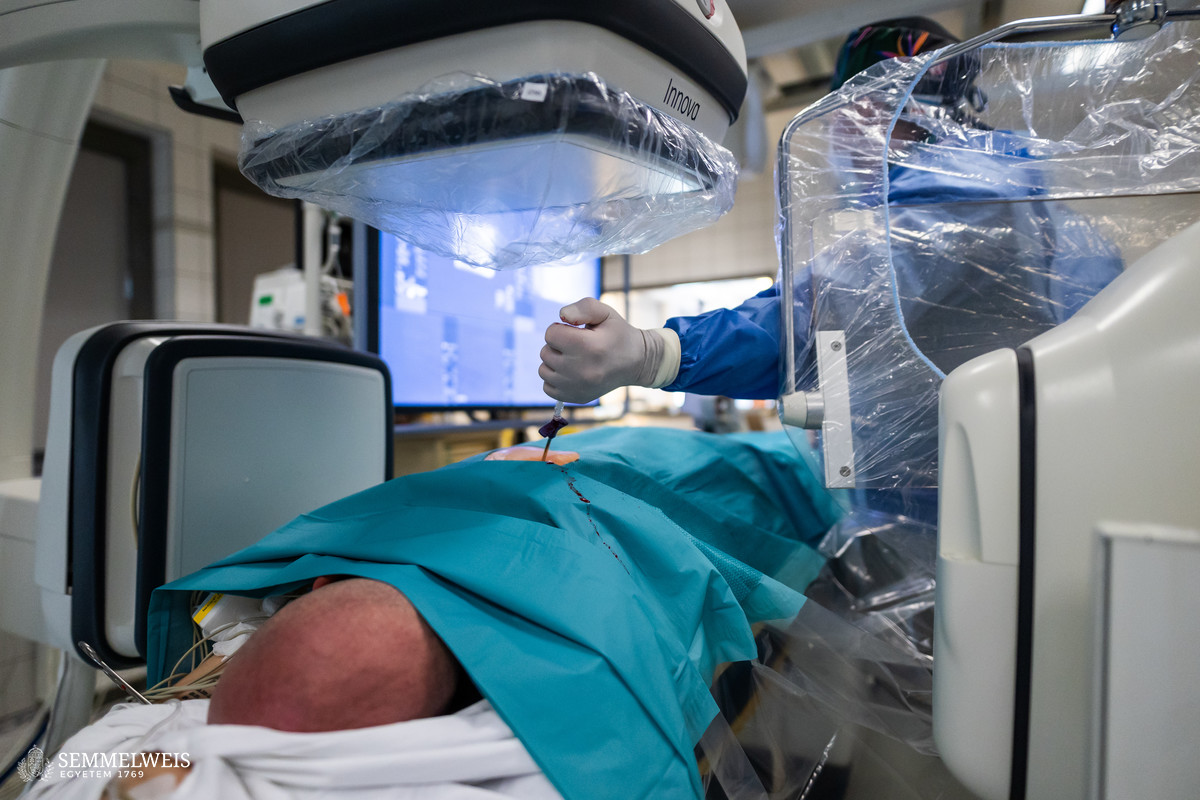
A young man treated for melanoma developed metastases affecting two vertebral bodies in the thoracic and lumbar regions, causing pain that impaired his quality of life and posed a threat of further neurological symptoms as the tumor progressed. In order to stop the underlying disease from advancing, to prevent neurological symptoms, and to reduce the patient’s pain, his doctors recommended radiofrequency ablation (RFA) treatment, said chief physician Dr. Sándor Nardai. He added that it was an internationally accepted, minimally invasive tumor management technique for the treatment of secondary vertebral tumors, mostly in cases where the extent of the disease or the patient’s general condition did not allow open spinal surgery. “The procedure involves puncturing the lesion with a thin needle, heating it up, and using the heat to destroy the abnormal cells. We then inject bone cement into the cavity to stabilize the vertebra to prevent any possible weakening of the vertebral statics,” explained Dr. Sándor Nardai.
The procedure can also include biopsy bone sampling, so three activities are performed in one operation: tumor treatment, spine stabilization, and diagnostic sampling.
In the long term, the intervention can effectively reduce the pain that impairs quality of life and affects basic activities, thus helping the patient to regain daily mobility and return to work. In addition, the progression of the tumor in the targeted region can be inhibited with good efficacy and further neurological damage can be prevented. The surgery was successful, and the patient was discharged home following 72 hours of observation.
Bone metastases develop in 30-75 percent of cancers, with 5-30 percent of these being vertebral metastases. Spinal metastases are most often caused by tumors of the breast, lungs, prostate, kidneys, colon (colorectal), and thyroid gland. In each case, treatment requires an individual assessment and the decision of the team treating the patient. Open spine surgery, RFA, radiotherapy, and oncological treatment constitute the repertoire from which the most appropriate treatment technique for the patient should be chosen. RFA can be used mainly as an alternative to radiotherapy and as an adjunct to open surgery.
In Hungary, RFA is a well-established, professionally approved procedure subject to the principle of equity, mostly used in the treatment of lung and liver metastases. Under the supervision of Dr. Zsolt Berentei, neuroradiology consultant at the Department of Neurosurgery and Neurointervention, which has recently merged with Semmelweis University, the first such intervention was performed in April for a lesion involving a vertebra. The demonstration surgery was supervised by Dr. Árpád Viola, head neurosurgeon at the Dr. Manninger Jenő Traumatology Center in Budapest, in the presence of Dr. Péter Banczerowski, Head of the Department of Neurosurgery. Since then, at the beginning of June, another patient was successfully treated with this technique. Dr. Sándor Nardai expressed his hope that more and more patients with vertebral tumors will benefit from this procedure. “We perform around 30-50 open spinal surgeries for vertebral metastases every year. Given the high incidence of spinal metastases and the prolonged survival following modern oncotherapy, this procedure can contribute to a better quality of life for many patients, either alone or in combination with open surgery or radiotherapy,” the chief physician concluded.
Eszter Keresztes
Translation: Judit Szabados-Dőtsch
Photos by Bálint Barta – Semmelweis University