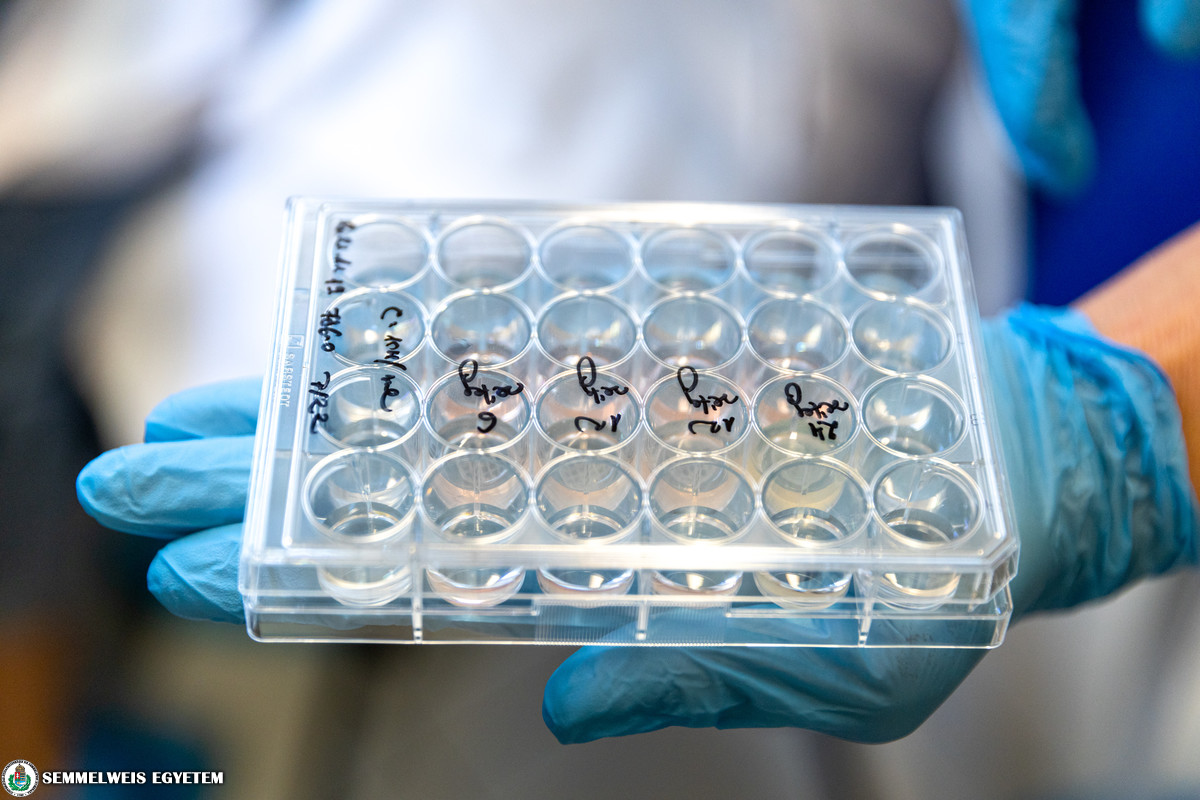
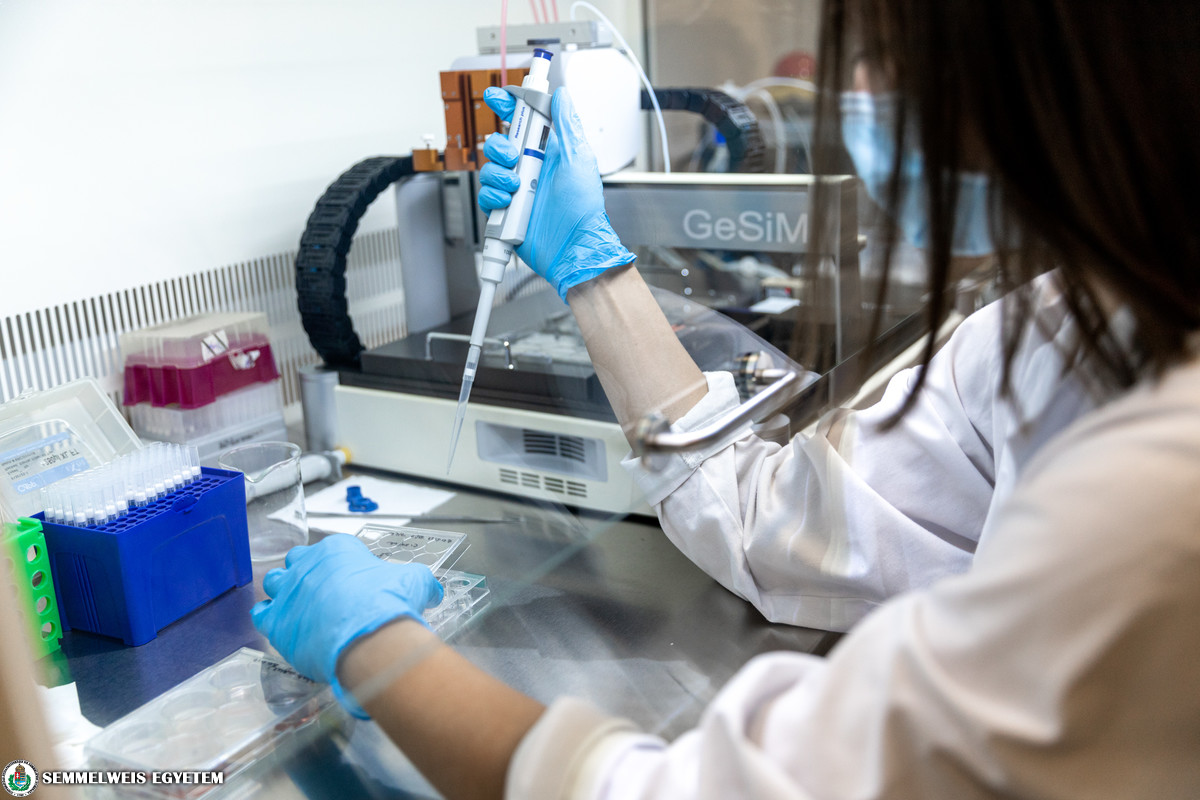
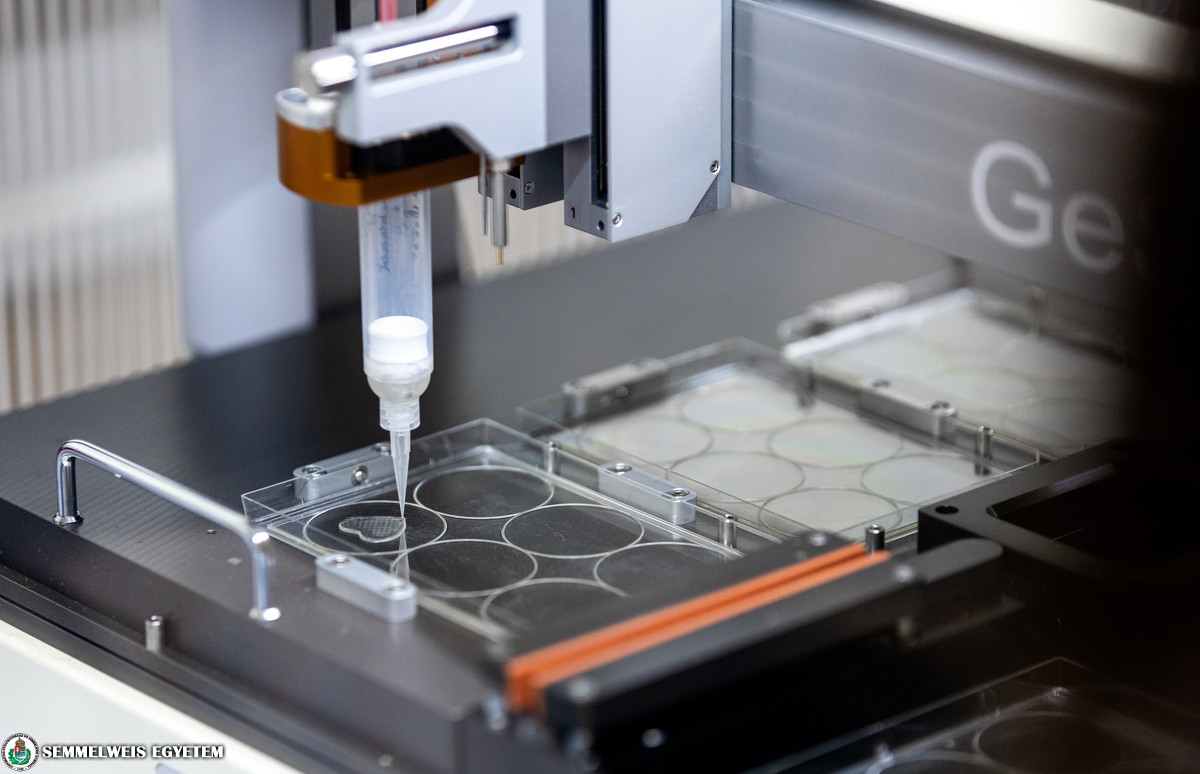
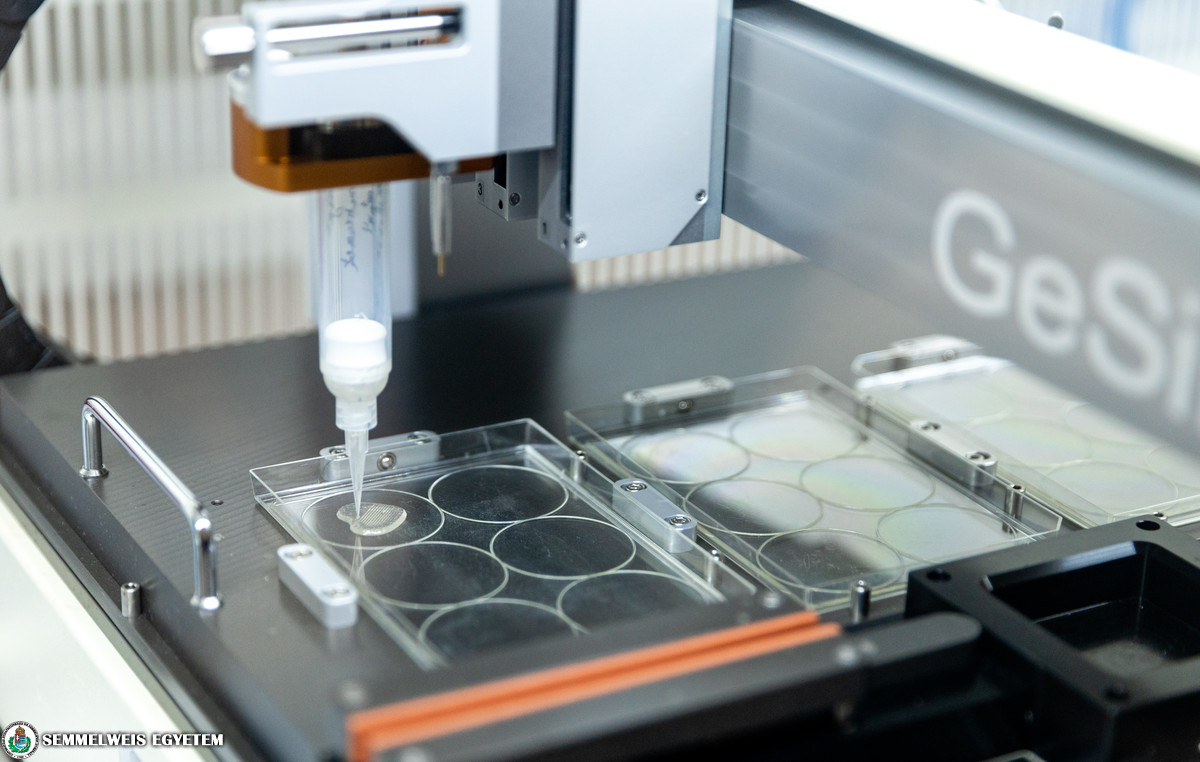
The Laboratory of Tumour Biology at the 1st Department of Pathology and Experimental Cancer Research Institute focuses on metabolic changes in tumours and their therapeutic inhibition. To produce bioink for 3D printing, tumour and other cells are isolated from tumour samples received at the institute using enzymes, then mixed with a gel-like matrix material. A special computer-controlled device can print complex tissue-like structures using multiple bioinks at once. Micrometre-precise bioprinting is assisted by compressed air pressure. By cross-linking the matrix material between cells, the printed structure can be stabilised to ensure that the pre-designed shape is maintained (e.g. vascular networks, small tissue discs, different cell layers, etc.). Culture medium is added to the printed structure, and then after a few days, or maybe a few weeks of culture, models of cell-cell interactions similar to real tissues are formed. In general, large numbers of tumour and other cells can be isolated from a small piece of tumour tissue, so many small tissue models of any shape, capable of growing in vitro, can be printed from bioinks containing different cells. These can be used in a wide range of studies, such as testing potential anti-tumour agents or targeted treatments emerging after modern molecular diagnostic procedures. The results can be used not only for basic research projects, but also for planning personalised treatments with more accuracy in the future. Tests that could be developed using the printing process would allow the design of a personalised treatment plan, including drugs selected specifically for the tumour, to be set up at the time of diagnosis. The introduction of this application requires the development of tailored protocols, which are currently being tested on animal tumour tissue samples. Upon a completion of that, testing of the technology in surgical tumours can begin.
The Laboratory of Tumour Biology at the 1st Department of Pathology and Experimental Cancer Research Institute focuses on metabolic changes in tumours and their therapeutic inhibition. To produce bioink for 3D printing, tumour and other cells are isolated from tumour samples received at the institute using enzymes, then mixed with a gel-like matrix material. A special computer-controlled device can print complex tissue-like structures using multiple bioinks at once. Micrometre-precise bioprinting is assisted by compressed air pressure. By cross-linking the matrix material between cells, the printed structure can be stabilised to ensure that the pre-designed shape is maintained (e.g. vascular networks, small tissue discs, different cell layers, etc.). Culture medium is added to the printed structure, and then after a few days, or maybe a few weeks of culture, models of cell-cell interactions similar to real tissues are formed. In general, large numbers of tumour and other cells can be isolated from a small piece of tumour tissue, so many small tissue models of any shape, capable of growing in vitro, can be printed from bioinks containing different cells. These can be used in a wide range of studies, such as testing potential anti-tumour agents or targeted treatments emerging after modern molecular diagnostic procedures. The results can be used not only for basic research projects, but also for planning personalised treatments with more accuracy in the future. Tests that could be developed using the printing process would allow the design of a personalised treatment plan, including drugs selected specifically for the tumour, to be set up at the time of diagnosis. The introduction of this application requires the development of tailored protocols, which are currently being tested on animal tumour tissue samples. Upon a completion of that, testing of the technology in surgical tumours can begin.
Altogether, more than 200 human tumour cell lines are available in the institute’s cell bank. We have started testing the most relevant tumour cells concerning public health – we are printing 3D tissue-like structures from breast and lung tumour cells, and testing the printing process with colon cancer and kidney tumour cells”
– explained Dr. Anna Sebestyén, Senior Research Fellow at the 1st Department of Pathology and Experimental Cancer Research, Head of the Tissue and Cell Culture Laboratory.
The Online Core Facility system at Semmelweis University
The living cell 3D bionic printer structure is now available in the online Core Facility system of Semmelweis University. This includes tools and services that are not only available to university researchers, but also to external researchers for industrial or academic use, upon a service fee or on a collaborative basis.
In this series of articles, we introduce the new research infrastructures to be included in the Core Facility system of Semmelweis University. The Core Facilily website is currently accessible via the internal university network. As soon as these services are available to external partners, this menu item will also be searchable from the public online interface.
 Treating a tumour is a big challenge. The tumour is constantly changing during interventions, medication and progression. Tissues created with 3D bionic printing, complemented with special microfluidics systems, could be used to model this in the future. Long-lasting 3D tissue-like structures can be used to study how aggressive tumour cell clones are selected out, and how certain tumours become resistant to treatment. Furthermore, the advantages of 3D models can be exploited in drug development as well: new, potential anti-tumour agents can be tested much more efficiently under these conditions than in 2D cell cultures. “Of course, these new types of studies cannot replace executive clinical trials and preventative animal testings, but they can reduce the number of animal experiments and failed phase studies, as they contribute to better select the drugs that are likely to be effective. This could also reduce the high costs of current drug development trials in the future,” she added.
Treating a tumour is a big challenge. The tumour is constantly changing during interventions, medication and progression. Tissues created with 3D bionic printing, complemented with special microfluidics systems, could be used to model this in the future. Long-lasting 3D tissue-like structures can be used to study how aggressive tumour cell clones are selected out, and how certain tumours become resistant to treatment. Furthermore, the advantages of 3D models can be exploited in drug development as well: new, potential anti-tumour agents can be tested much more efficiently under these conditions than in 2D cell cultures. “Of course, these new types of studies cannot replace executive clinical trials and preventative animal testings, but they can reduce the number of animal experiments and failed phase studies, as they contribute to better select the drugs that are likely to be effective. This could also reduce the high costs of current drug development trials in the future,” she added.Translation: Viktória Kiss
Photo: Attila Kovács – Semmelweis University