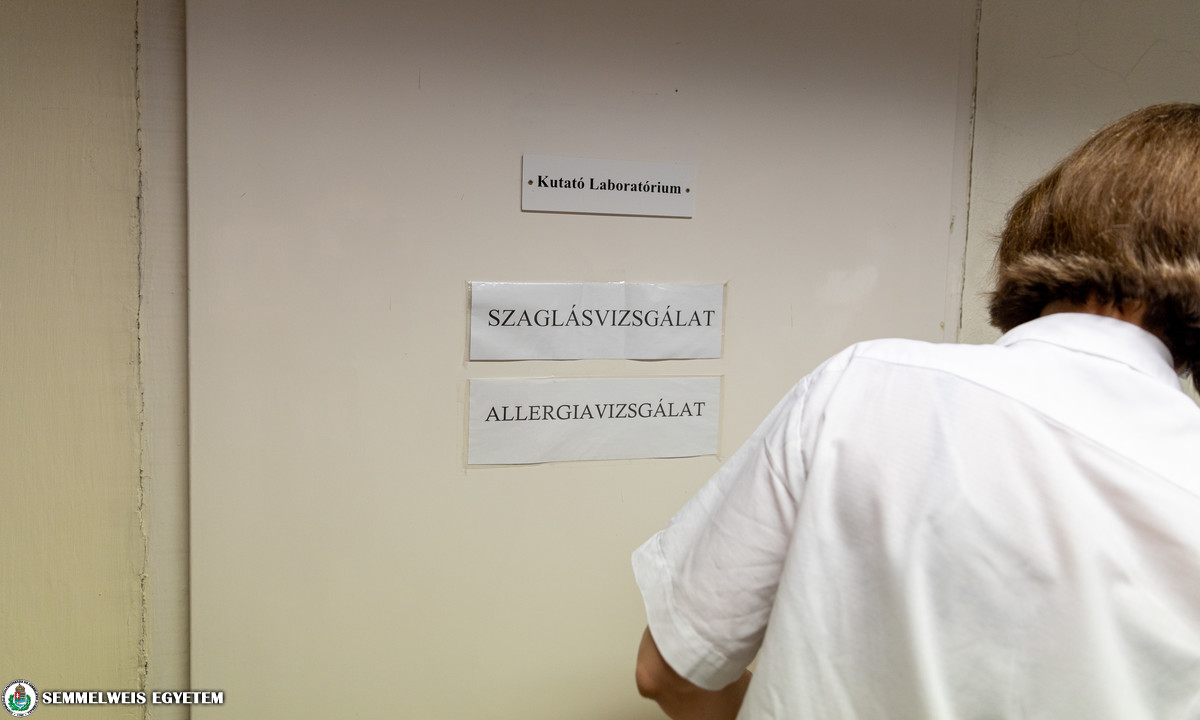
Semmelweis University’s Department of Otorhinolaryngology, Head and Neck Surgery has just started the operation of its post-COVID Outpatient Clinic for Olfactory Disorders, where such patients are being treated with olfactory testing and olfactory training, who have had complaints related to the loss of smell or a reduced/changed sense of smell for more than three weeks after a coronavirus infection. It is the first olfactory examination center in Hungary.
“The complete loss of smell, anosmia and the change in the sense of smell have been pre-existing problems, but the number of people with these complaints has increased due to the coronavirus. In the case of many patients, this is the first or, in some cases, the only symptom of the coronavirus infection. However, there is also a large number of people whose complaints remain after the illness, too”, said Dr. László Tamás, Head of the Department of Otorhinolaryngology, Head and Neck Surgery.
“More and more patients have reported that their sense of smell has changed: it was either a complete loss of smell, or when the sense of smell is changed. In addition, many people complained about starting to smell unpleasant odors. Both phenomena need to be medically examined if they last longer than 3 weeks”, the department head highlighted.
Dr. László Tamás emphasized that the department has been involved in the fight against the coronavirus and in COVID-care, but due to the reduction in the number of infected patients, the planned treatments have been restarted at the department and the post-COVID Outpatient Clinic for Olfactory Disorders has also started operating. He also added that the department had offered treatment opportunities for patients with olfactory complaints for years.
“The coronavirus has only reassured us of the need for such care”, the department head said.
The number of patients with olfactory complaints has increased at an unprecedented rate during the pandemic, therefore the Outpatient Clinic for Olfactory Disorders currently operates mainly as a post-COVID care unit.
 “It is not yet known for sure why a coronavirus infection causes amnosia. The virus appears to stick to the nasal and nasopharyngeal mucosa, which can lead to the damage of olfactory receptor cells. It is likely that the virus does not act directly on the receptor cells, but rather they are damaged due to the death of the surrounding cells. This can result in the fact that the first symptom is amnosia in the case of many patients. According to another theory, the infection attacks the olfactory tracts when it enters the nervous system, but the results so far tend to support the former theory. The so-called olfactory training may provide support for patients having such complaints in restoring their sense of smell”, Dr. László Tamás explained.
“It is not yet known for sure why a coronavirus infection causes amnosia. The virus appears to stick to the nasal and nasopharyngeal mucosa, which can lead to the damage of olfactory receptor cells. It is likely that the virus does not act directly on the receptor cells, but rather they are damaged due to the death of the surrounding cells. This can result in the fact that the first symptom is amnosia in the case of many patients. According to another theory, the infection attacks the olfactory tracts when it enters the nervous system, but the results so far tend to support the former theory. The so-called olfactory training may provide support for patients having such complaints in restoring their sense of smell”, Dr. László Tamás explained.
The Outpatient Clinic for Olfactory Disorders at the Department of Otorhinolaryngology, Head and Neck Surgery is the first olfactory examination center in the country. According to Dr. Helga Kraxner, head of the outpatient clinic, there may be several factors behind the loss of smell or the changed sense of smell.
“It is possible that someone’s olfactory disorders are due to a trauma, or happens after a surgery, and it may be caused by a neurodegenerative disease, a medicine, or just some sort of an infection”, Dr. Helga Kraxner said.
 As she pointed out, most commonly those patients report about this problem, who have suffered from a coronavirus infection with such symptoms, therefore the outpatient clinic currently operates primarily as a post-COVID care unit. Dr. Helga Kraxner emphasized that just like the infection itself, its symptoms related to smell may occur in countless forms. In addition to the changed sense of smell, parosmia may also occur, when the person smells inappropriate odors and phantosmia (phantom smell), too. Some people have symptoms that disappear after a few days, but it may also happen that these symptoms become persistent and remain even after the infection is over. According to the head of the outpatient clinic, if the loss of smell or the change in the sense of smell persists for more than 3 weeks, it is advisable to consult a doctor.
As she pointed out, most commonly those patients report about this problem, who have suffered from a coronavirus infection with such symptoms, therefore the outpatient clinic currently operates primarily as a post-COVID care unit. Dr. Helga Kraxner emphasized that just like the infection itself, its symptoms related to smell may occur in countless forms. In addition to the changed sense of smell, parosmia may also occur, when the person smells inappropriate odors and phantosmia (phantom smell), too. Some people have symptoms that disappear after a few days, but it may also happen that these symptoms become persistent and remain even after the infection is over. According to the head of the outpatient clinic, if the loss of smell or the change in the sense of smell persists for more than 3 weeks, it is advisable to consult a doctor.
For the time being, the Outpatient Clinic for Olfactory Disorders at the Department of Otorhinolaryngology, Head and Neck Surgery receives patients three times a week, on Tuesdays, Wednesdays and Thursdays, but the consultation hours may be extended if necessary. The Outpatient Clinic for Olfactory Disorders is available for patients who are having a GP referral or a referral from an otorhinolaryngology outpatient clinic. In addition, the university’s post-COVID units may also send patients here.
According to Dr. Helga Kraxner, in the case of post-COVID amnosia and amnosia of any other origin, the first step is always a detailed otorhinolaryngology examination. This is performed to assess whether there is a mechanical barrier (swelling of the nasal mucosa, chronic sinusitis, nasal polyps or some other types of lesion) that has worsened the sense of smell because the air does not reach the olfactory epithelium. For this purpose, an endoscopic examination, and if necessary, an imaging examination (CT or MR) are also performed. It is also possible that the change in the sense of smell occurs due to an allergy, therefore a differential diagnosis of this may be needed. The latter is also performed at the department’s Outpatient Clinic for Allergology, by prior appointment. Dr. Helga Kraxner highlighted that in case the anamnesis indicates the existence of other problems, they may also refer the patient to consult other specialists, too, for example at the neurological outpatient clinic.
As Dr. Helga Kraxner pointed out, if a lesion requiring current otorhinolaryngology treatment is not found in the background of amnosia, an olfactory test is carried out. With the help of the complex measuring device used at the Outpatient Clinic for Olfactory Disorders, odor detection threshold, odor discrimination and odor identification are also examined. After an examination of approximately 45 minutes, each patient receives a TDI (Threshold, Discrimination, Identification) score, which is used to classify whether the patient have a normal sense of smell, a reduced sense of smell, or have lost his/her sense of smell. In the latter two cases, olfactory training is recommended for the patient. At the end of the planned training period, a repeated test is performed to evaluate the therapeutic outcome.
“The essence of olfactory training is that the patient smells concentrated scents such as floral, spicy or fruity scents in a concentrated manner twice a day for a minimum of 12 weeks, recalling their original feeling. They should concentrate on each scent for 10-20 seconds and then recall feelings about it based on past memories. It is also recommended to keep an olfactory diary, in which the patient evaluates his/her own sense of smell on a scale once a week, always at the same time”, Dr. Helga Kraxner highlighted.
Based on their experiences so far, olfactory training may significantly improve the condition, or even restore the sense of smell. There have been positive experiences in connection with reduced sense of smell of other origins (traumatic, viral or of unknown origin) as well, and the method also seems to be effective for reduced sense of smell induced by the novel type of coronavirus. However, in order to achieve a good result, it is important for patients to see a physician if they have any complaints and to start the treatment as soon as possible. In addition to olfactory training, other therapies are also being used, if necessary, such as steroid nasal sprays or hyaluronic acid sprays for topical treatment, or nasal drops containing vitamin A.
Ádám Szabó
Photo: Attila Kovács – Semmelweis University
Translation: Katalin Illés-Romhányi