At Semmelweis University, the 1st Department of Pediatrics is the designated COVID patient care provider for the treatment of COVID-19 patients under the age of 18 years. In children, coronavirus infection typically causes milder symptoms, therefore the department’s COVID care unit with 15 beds operated at nearly full capacity only at the peak of the third wave of the epidemic. However, it is a serious challenge regarding this age group that general pediatric symptoms have a strong resemblance to coronavirus infection. We asked Dr. Attila Szabó, Department Head, Director of the Clinical Center, and Anita Czira, Head Nurse of the department about their experiences related to COVID-19.
“Teamwork and collaboration have never been so strong”
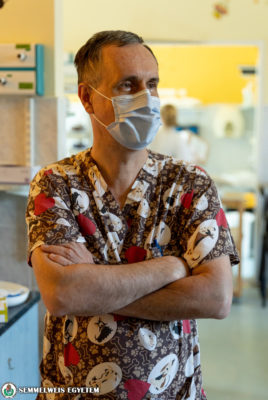
Dr. Attila Szabó, Department Head, 1st Department of Pediatrics
How long have you been involved in COVID patient care? Do you remember the first case?
 The situation of pediatrics is special in that, although COVID-19 can severely affect people under the age of 18, yet the infection is mostly milder, and often asymptomatic in this age group. However, there are some COVID-positive children who need hospital treatment either directly because of the infection or because of their underlying disease. Since 20 March 2020, we have operated a COVID unit at the department, as well as a separate unit where suspected COVID-19 cases are admitted until the test results are available. The latter, which is also called the gray zone, is busier than the red zone. General pediatric problems (fever, cough, abdominal complaints) which patients have at the time of admission to our department are very similar to the symptoms of COVID-19, therefore practically most of them were/are admitted through the intermediary unit. Abdominal complaints are much more common in case of children with coronavirus infection than in the case of adults. Pediatric patients may even produce symptoms similar to appendicitis. I exactly remember the first COVID-positive case, because we had to treat the affected child in an intensive care unit on a ventilator for a few days, fortunately successfully. It was later revealed that the severe complaints were not directly caused by the coronavirus infection but by the child’s underlying disease.
The situation of pediatrics is special in that, although COVID-19 can severely affect people under the age of 18, yet the infection is mostly milder, and often asymptomatic in this age group. However, there are some COVID-positive children who need hospital treatment either directly because of the infection or because of their underlying disease. Since 20 March 2020, we have operated a COVID unit at the department, as well as a separate unit where suspected COVID-19 cases are admitted until the test results are available. The latter, which is also called the gray zone, is busier than the red zone. General pediatric problems (fever, cough, abdominal complaints) which patients have at the time of admission to our department are very similar to the symptoms of COVID-19, therefore practically most of them were/are admitted through the intermediary unit. Abdominal complaints are much more common in case of children with coronavirus infection than in the case of adults. Pediatric patients may even produce symptoms similar to appendicitis. I exactly remember the first COVID-positive case, because we had to treat the affected child in an intensive care unit on a ventilator for a few days, fortunately successfully. It was later revealed that the severe complaints were not directly caused by the coronavirus infection but by the child’s underlying disease.
What is the role of your unit in COVID-19 patient care?
Within Semmelweis University, the 1st Department of Pediatrics is the designated COVID care provider for children under 18. One of the reasons for this is that it is close to the Outer Clinical Block providing COVID care, but we have also taken the the 2nd Department of Pediatrics into consideration, where patients of hematooncology are treated, who are particularly exposed to infections. During the epidemic we were lucky to have three separate pavilions at our department, becauase we could manage affected patients. The pavilions were built a long time ago to isolate infectious patients.
To what extent did you have to reorganize work?
By 20 May 2021, we had treated a total of 103 COVID-positive patients at our department. Therefore, it can be seen that the number of pediatric cases is not comparable to that of adult patient care, yet we had to completely reorganize our activities. Patients arrive at the department through the pediatric emergency department, which also serves as a screening gate in an epidemiological situation, and the colleagues working here perform the primary diagnostics dressed in protective equipment. The COVID unit was established in our building, where previously patients with renal diseases were treated. These patients and others with problems independent of the coronavirus were transferred to the main building. The grey zone was also set up in a separate pavilion. Basically, the same colleagues provide patient care at both the gray and red zones from the very beginning, but the low number of cases also allowed us to help other units: 27 of our staff members were working in COVID care provided by other departments at the university.
As far as pediatric care is concerned, what differences do you see between the different waves of the epidemic at the department?
The first wave was the time for preparations due to the low number of cases. We placed a special emphasis on teaching the use of protective equipment and provided PCR screenings not only to our patients, but also to accompanying parents. During the second wave, the number of cases had already increased, but it only happened during the third wave that our 15-bed COVID unit had to operate at almost full capacity. At the same time, the specialty of pediatric care is that in the epidemic situation, we also made sure that one of the parents could stay with their child, even at the COVID unit, and the majority of parents used this opportunity. In addition, the department participates in the vaccination program, and we run a separate vaccination point. Furthermore, we also treated a low number of newborns infected with coronavirus in our preterm intensive care unit.
What are the most important lessons and experiences that will be useful in the future?
Over the past year, we have been able to quickly find answers, learn new things, and adapt effectively even to the most unexpected situations, not only at the level of the department, but also at the level of the university. Teamwork and collaboration have never been so strong. The pandemic is a common threat that arch over disciplines and everyone was looking for solutions and not problems. We may say that the common enemy has brought people together. In addition, the epidemic also resulted in the establishment of a separate unit for the care of infectious diseases at our department, which we will maintain in the future, thus enriching the portfolio of our clinic.
“We should be present by the children’s hospital bed in a way that makes them feel safe”
Anita Czira, Head Nurse, 1st Department of Pediatrics
In terms of professional and nursing responsibilities, what is the biggest change that the coronavirus has brought?
 Work has not changed significantly, but due to the circumstances, the processes have to be carried out differently, which of course has a repercussion on the entire patient care. The main challenge was how we could perform the same tasks in accordance with epidemiological measures. This period has taught us a great deal. One of the most important lessons is the optimization and practical grouping of the processes. In case of isolated patient care, prioritization of the activities and the use of a checklist have been more important than ever. For example, if we leave something outside the red zone, in the current situation this means taking off the protective equipment and putting it on again. In the isolated wards, we also had to create the right conditions for various diagnostic and therapeutic services, such as adequate lighting for taking blood samples. Many patients were admitted to the COVID unit, because they had had surgery earlier, but they also turned out to have a positive COVID test result. In their case, conditions had to be created for surgical aftercare in the ward of the red zone, too, as we could not move them outside. Our ability to continually adapt has improved a great deal in the recent period. Each day, we had to deal with another challenge and these skills will also remain with us when the epidemic is over.
Work has not changed significantly, but due to the circumstances, the processes have to be carried out differently, which of course has a repercussion on the entire patient care. The main challenge was how we could perform the same tasks in accordance with epidemiological measures. This period has taught us a great deal. One of the most important lessons is the optimization and practical grouping of the processes. In case of isolated patient care, prioritization of the activities and the use of a checklist have been more important than ever. For example, if we leave something outside the red zone, in the current situation this means taking off the protective equipment and putting it on again. In the isolated wards, we also had to create the right conditions for various diagnostic and therapeutic services, such as adequate lighting for taking blood samples. Many patients were admitted to the COVID unit, because they had had surgery earlier, but they also turned out to have a positive COVID test result. In their case, conditions had to be created for surgical aftercare in the ward of the red zone, too, as we could not move them outside. Our ability to continually adapt has improved a great deal in the recent period. Each day, we had to deal with another challenge and these skills will also remain with us when the epidemic is over.
To what extent do these pediatric patients require special nursing care?
In case of pediatric care, communication always receives special attention, it is essential to make children trust us. Wearing the protective equipment required in an epidemiological situation is often frightening, for adults as well, and this is even more so in case of children. For this reason, patient care in protective equipment requires a lot of creativity: we have supplemented the communication channels with an online solution, and we pay special attention to have as many direct, human gestures as possible. We should be present by the children’s hospital bed in a way that makes them feel safe.
How did you ensure the presence of a parent, legal representative in pediatric care during the ban from hospital visits?
One of the specialties of pediatric COVID care is that one of the parents may stay with the child in the ward, which is as much a part of everyday life during the pandemic as it is so during other times as well. This is definitely a plus, as the presence of a parent provides assistance in pediatric care. In addition, the parent knows the child the best and quickly detects any changes in his/her condition. We have always worked with the parent as a team, but during the epidemic, the role of this collaboration has been further reinforced. We paid special attention to the continuous communication and consultation opportunities for the parent in the isolated ward, including the possibility of telephone and video calls. Even in this situation of uncertainty, raised by anxiety about the child, it is particularly important to use all tools that help build confidence. At the same time, all this required more attention and observation on our part.
What are the most important lessons and experiences that will be useful in the future?
The increased role of checklists, the complementary use of online communication tools are all important aspects that will be incorporated into our everyday lives in the future as well. However, if I had to sum it up in one word, I would mention cohesion as the most important experience. I am proud to work with colleagues who have held on in the challenging situation, pushing the boundaries of human power to achieve a common goal. Without all this, we would not have been able to run our COVID unit and intermediary unit at a high standard in addition to providing general pediatric care and operating both the outpatient clinic for long COVID symptoms and our vaccination point without interruption.
Pálma Dobozi
Photo: Attila Kovács – Semmelweis University
Translation: Katalin Illés-Romhányi





