The Medical Imaging Center has been involved in COVID care since the infection appeared in Hungary, as they provide an essential diagnostic background in patient care. Coming up next in our series of articles presenting the organizational units involved in COVID care, Dr. Pál Maurovich-Horvat, Director talks about his experiences.
How long have you been involved in COVID patient care? Do you remember the first case?
 As an organizational unit dealing with diagnostics, the Medical Imaging Centre has been engaged in COVID care since the appearance of the virus in Hungary. I clearly remember the first CT image that showed the characteristic pattern of pneumonia typical of coronavirus. It was taken of a young male patient, who was brought to our center from the Emergency Department in March 2020. At that time, the disease was still considered rare, we only heard about the coronavirus based on information from hospitals abroad and on the Internet.
As an organizational unit dealing with diagnostics, the Medical Imaging Centre has been engaged in COVID care since the appearance of the virus in Hungary. I clearly remember the first CT image that showed the characteristic pattern of pneumonia typical of coronavirus. It was taken of a young male patient, who was brought to our center from the Emergency Department in March 2020. At that time, the disease was still considered rare, we only heard about the coronavirus based on information from hospitals abroad and on the Internet.
What is the role of your unit within the university in COVID-19 patient care?
The Medical Imaging Center provides the diagnostic background for the Emergency Department and the entire Outer Clinical Block. Since one of the most common complications of COVID-19 is pneumonia, diagnostics, especially CT, is particularly important in COVID-19 care. When the virus appeared, we developed a parallel diagnostic process and patient care: normal, green-zone, and red-zone radiology for coronavirus diseases are safely performed.
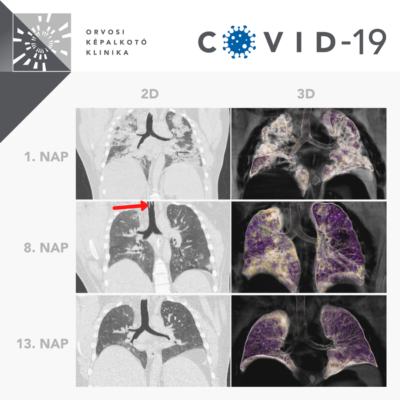
At the university, at least one X-ray image is made of every patient suspected of COVID infection, and a CT scan if the suspicion of the infection is confirmed. These images clearly show the pneumonia caused by the coronavirus and the extent of the inflammation can also be estimated. Follow-up is usually done with a CT to monitor the efficiency of the therapy, but the patient’s condition is a determining factor in what imaging procedures we use.
As far as the center is concerned, how do you see the difference between the first, the second, and the current, third wave?
In terms of tools and equipment, we were expecting the second and third waves with a reinforced arsenal: we replaced our 16-slice CT device with a more modern, 128-slice CT scan, and we also acquired a high-tech robotic X-ray and ultrasound equipment. We desperately needed all of this, as the second wave has put much more workload on health care and patient care at Semmelweis University as well. There were more patients in serious condition during the second wave, and since then it has been proven that COVID also increased the number of thromboembolic abnormalities and strokes: this is what we also experienced at the Department of Emergency Radiology. The self-propelled disinfectant robot procured from Denmark with the support of the university and 77 Elektronika Kft. provides great help to us. Thanks to this device, the specialists of the Medical Imaging Centre were not infected by the virus during the first two waves. Now, in the third wave, the load is expected to be even larger. We started to use new mobile X-rays, and a few weeks ago we also handed over a modern 128-slice CT device at the Department of Pulmonology. We recently exceeded 120 acute CT scans performed in one day. This means that there are periods when a new CT scan is initiated every 3-5 minutes. To achieve such performance the work of excellent health care professionals and physicians is also required in addition to the state-of-the-art equipment. However, due to the vaccination of those involved in patient care, our staff are at less risk.
How did you have to reorganize work?
Significant reorganization was required, shifts with compensatory time were introduced and graduate education was largely transferred to an online platform. Fortunately, new methods, such as our teleradiology system, helped us with this. In addition, we paid attention to keeping distance, and when doing the medical records, we tried to separate the work processes in space and time. The Medical Imaging Centre is a relatively recent organizational unit, which had to face the challenges of the pandemic a few months after its establishment in 2019. However, I think that our three departments, the Department of Radiology, the Department of Nuclear Medicine, and the Department of Neuroradiology, worked together perfectly and we have always been able to provide support to each other.
What are the most important lessons and experiences that will be useful in the future?
The coronavirus has brought many changes that will remain with us even after the epidemic. The development of diagnostic algorithms based on artificial intelligence has greatly accelerated and our clinic is also involved in this. Together with a research team in Los Angeles we developed an artificial intelligence-based platform to quantify the severity of COVID-induced pneumonia that can predict with high accuracy who will need ventilation and the likelihood of a poor outcome of the disease. In addition, we also took part in the development of applications for stroke diagnostics based on a similar principle, or research on platforms for the detection of lung nodules together with a Hungarian consortium. The Medical Imaging Centre has also undergone a number of improvements: we have set up an epidemiologically safe reception desk and renovated the inner courtyards with university support. In this project, we set up smart tables, creating modern community spaces in the Central Patient Care Building that can also be used as an outdoor classroom, making it safer to hold practical sessions, to have consultations and conversations outdoors. We also tried to make the Outer Clinical Block more student-friendly. Perhaps the most positive change is that we launched a series of morning lectures last semester. Due to the epidemic, the official morning discussions and the subsequent lectures were organized online through Zoom. We thought that we would make these contents available for every Hungarian resident even to those across the border. Since then, many residents have started their day with the “resident radio” of the Medical Imaging Centre at 8:05 a.m. The 20-25-minute-long lectures are grouped around one topic each week, following the curriculum of the European Society of Radiology. Based on the positive feedback, we plan to continue this online training even after the epidemic.
Ádám Szabó
Photo: Attila Kovács – Semmelweis University; Semmelweis University, Medical Imaging Centre Facebook page
Translation: Katalin Illés-Romhányi












