In his closing speech at the Basic Medical Science Center, Dr. Béla Merkely, Rector of Semmelweis University, pointed out that the Semmelweis Symposium not only demonstrated the high regard in which medical and health sciences were held at the institution; it also proved the everyday commitment of Semmelweis Citizens to their patients, healthcare in Hungary, and the advancement of science. He reminded the audience that the university’s most prestigious international scientific event had been held since 1992 but had never been as grand as this year: “Over three days, we welcomed more than 1,200 participants at our two venues, who were able to listen to 86 presentations and take part in five workshops. A total of 59 international speakers from 26 countries have visited us – representing our region, Central and Eastern Europe, as well as the United States, China, Singapore, and many other countries. They truly belong to the cream of the crop in their profession,” he said.
Our namesake, Ignác Semmelweis, one of the world’s most famous doctors, the “Savior of Mothers,” taught us never to be satisfied with merely doing our duties, but always to strive for more and better. It is thanks to this that our institution has become one of the world’s leading medical and health sciences universities, consistently ranking among the top 300. And this has also inspired our symposium, which now has more than three decades of history. – Dr. Béla Merkely
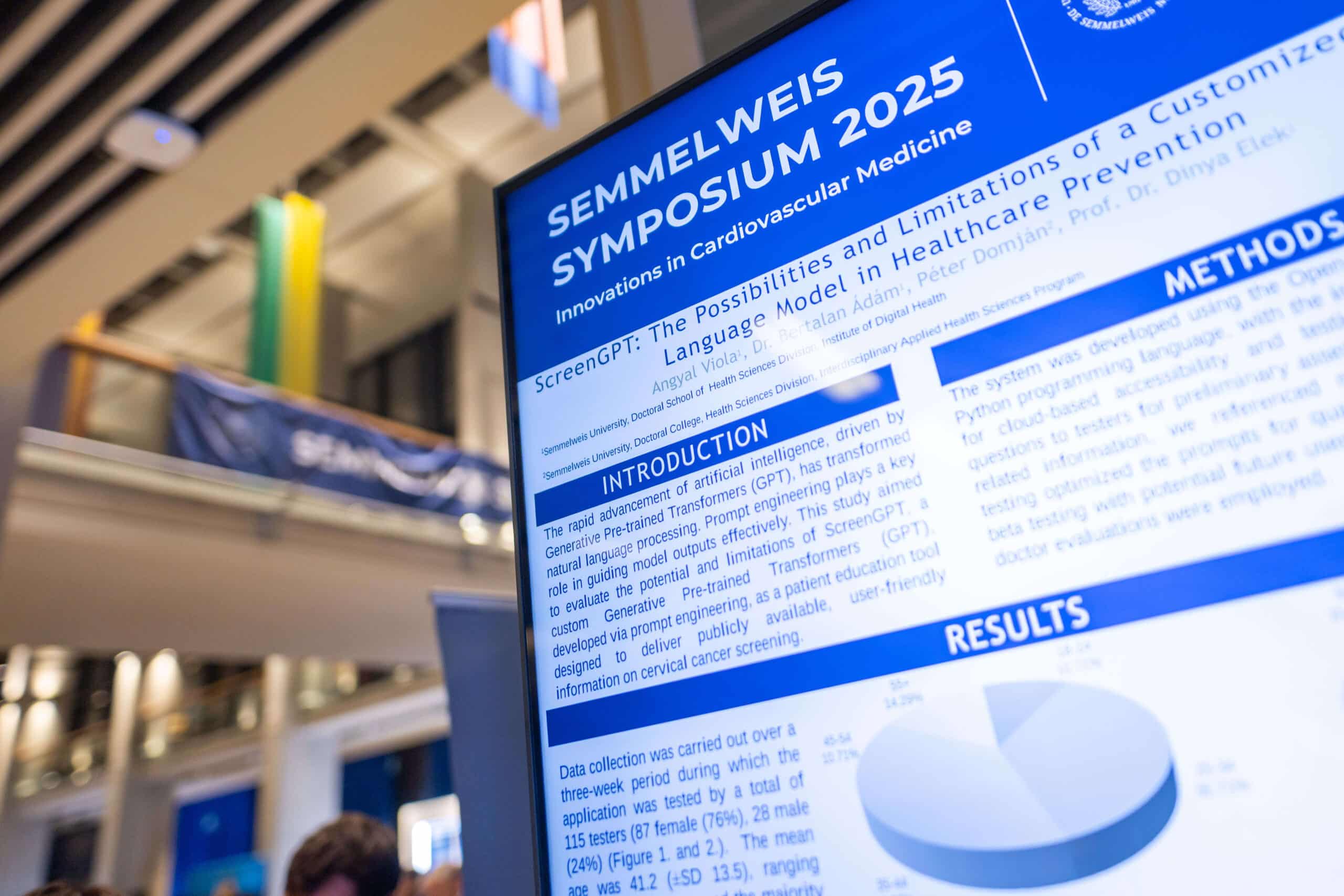
The 2025 Semmelweis Symposium focused on the latest advances and clinical practices in cardiovascular medicine, encompassing a wide range of topics from myocardial diseases, heart failure, vascular surgery, and imaging technologies to procedures such as cardiac transplantation and electrophysiology. It also highlighted emerging fields such as cardiovascular immunology, oncocardiology, sports cardiology, and space medicine, emphasizing interdisciplinary collaboration and cutting-edge research to improve cardiovascular health and treatment outcomes.
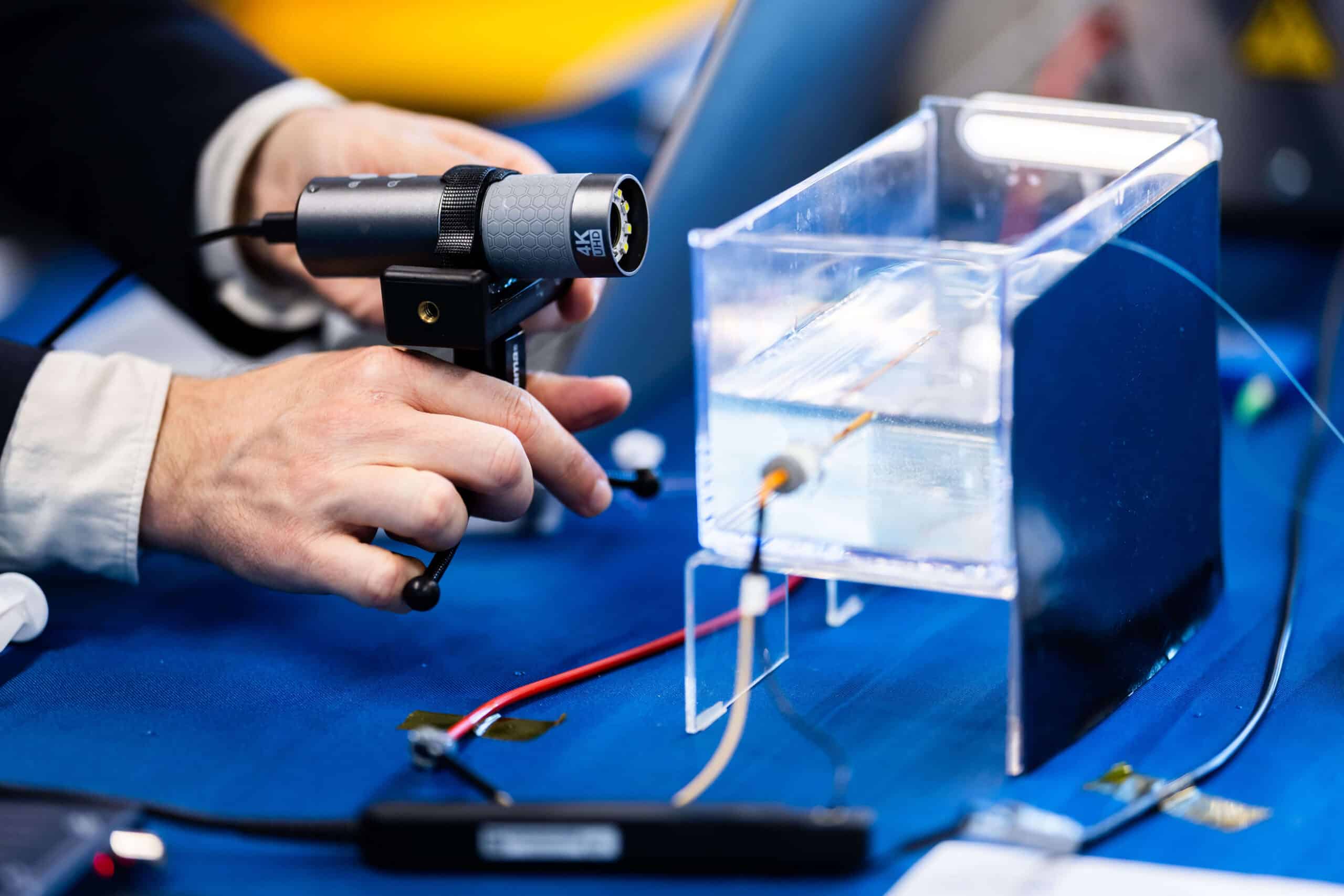
As part of the program, five workshops were held in addition to the theoretical sessions. The workshops focused on stress tests in cardiology, 3D echocardiography, pulsed-field ablation (Beat AF study), as well as cardiovascular imaging (CCTA, CMR, MRA); there was also a practical session that involved a guided visit to the Scientific Research Laboratory of the Városmajor Heart and Vascular Center. At the cardiopulmonary exercise testing workshop (Stress Tests in Cardiology), participants had the opportunity to observe the examination of a professional basketball player. The workshop was joined by Dr. Thomas G. Allison, Consultant in the Department of Cardiovascular Medicine and Cardiovascular Surgery and Professor of Medicine in the Mayo Clinic School of Medicine. He is one of the most iconic figures in exercise physiology, having analyzed close to 100,000 tests over nearly 50 years of professional experience, pointed out cardiologist and sports physician Dr. Nóra Sydó, Assistant Professor at the Városmajor Heart and Vascular Center. She learned all the elements of performing and evaluating cardiopulmonary exercise tests during her visits at the Mayo Clinic. Thanks to this experience, Semmelweis University’s Városmajor Heart and Vascular Center has been performing cardiopulmonary exercise tests at a high professional level similar to the Mayo Clinic for more than ten years.
A summary of individual sessions can be accessed by clicking on the names of the sessions below:
In the “Interdisciplinary Perspectives in Myocardial Diseases” session, myocardial diseases of different etiology were discussed. Understanding the mechanisms of myocardial injury, remodeling, and recovery requires collaboration across many disciplines.
Beyond the Hungarian professors of Semmelweis University, the organizers of the symposium had the great pleasure of welcoming two keynote lecturers: Dr. Jeanette Schulz-Menger (Germany) and Dr. Derek Hausenloy (Singapore).
Dr. Jeanette Schulz-Menger is a world-renowned cardiologist and CMR specialist and head of the Working Group on Cardiovascular Magnetic Resonance at Charité-Universitätsmedizin Berlin. She leads international initiatives that integrate imaging biomarkers into daily clinical decision-making. She delivered her presentation on “Cardiomyopathy Mindset and CMR,” highlighting cardiac magnetic resonance imaging as one of the most sophisticated imaging modalities in cardiology and playing a key role in diagnosis.
Dr. Derek Hausenloy is Director of the Cardiovascular and Metabolic Disorders Program at Duke-NUS Medical School. His groundbreaking research on cardioprotection and ischemia-reperfusion injury has uncovered mechanisms that protect the heart from cellular damage. Through global collaborations, he is advancing novel conditioning therapies and pharmacological interventions aimed at improving survival after acute myocardial infarction. In his lecture, he addressed the challenges and opportunities in cardioprotection against myocardial infarction and heart failure.
Dr. Hajnalka Vágó, Professor at the Városmajor Heart and Vascular Center
Dr. Kálmán Benke opened the session by emphasizing the importance of early recognition of Marfan syndrome and patient education, highlighting the role of the Hungarian Marfan Foundation and the VASCERN network, which enables access to high-level international care. Dr. Klaus Kallenbach presented the links between genetic background and clinical symptoms, which are essential for personalized therapy. He also introduced the PEARS procedure, where a custom external mesh supports the dilated aortic root without opening the aorta, reducing surgical risk and speeding recovery. Dr. Julie de Backer focused on cardiomyopathy associated with Marfan syndrome, noting that not only aortic rupture but also myocardial dysfunction represents a significant threat. Her team conducts animal studies to identify new therapeutic targets. Dr. Janine Meienberg highlighted the value of modern genomic techniques – especially whole-genome sequencing – in diagnosing hereditary aortic diseases. She emphasized studying the biomechanical effects of genetic variants and reported promising laboratory findings on celiprolol, which may improve the aortic wall’s resilience. Overall, the session showed that future Marfan care would integrate genetics, advanced imaging, innovative surgery, and preclinical research, moving strongly toward personalized medicine to improve patient safety and quality of life.
Dr. Kálmán Benke, Associate Professor at the Városmajor Heart and Vascular Center
The oncocardiology session presented the interconnection between cancer and cardiovascular damage in light of the latest research. Dr. Stefan D. Anker’s presentation described myocardial and weight loss in cancer patients as a complex heart failure syndrome, emphasizing the role of inflammatory and catabolic processes. Dr. Wouter Meijers presented the “reverse cardio-oncology” approach, according to which heart failure itself can increase the risk of malignant tumors; his presentation offered a new approach to the oncological screening of cardiology patients. In his video presentation, Dr. Tomas Neilan summarized the clinical challenges of myocarditis in the era of immune checkpoint inhibitors, highlighting the importance of imaging methods in early diagnosis. The session was concluded by Dr. Zsófia Drobni’s presentation, which provided practical guidance on the organization of oncocardiology care, risk-based monitoring, and multidisciplinary collaboration. During the panel discussion, the speakers explored the possibilities of domestic adaptation, the need for protocol development, and future research directions.
Text: Dr. Zsófia Dóra Drobni, Resident at the Városmajor Heart and Vascular Center; translation: Dr. Balázs Csizmadia
The session reviewed current and future perspectives in cardiac transplantation and mechanical circulatory support (MCS). Dr. Andreas Zuckermann discussed clinical usage of NMP (Normothermic Machine Perfusion) and HMP (Hypothermic Machine Perfusion) OCSs (Organ Care Systems), forecasting that organ preservation would become routine with global allocation systems enabled by OCS, alongside innovative methods to improve organ suitability through organ transformation for recipients. Dr. Jan Schmitto then highlighted “Beating Heart Implantation,” reducing ischemia/reperfusion injury with NMP OCS, and that the OCS Heart EXPAND Trial demonstrated success for the NMP method. The session also addressed Heart Mate III LVAD long-term treatment outcomes for advanced heart failure, presented by Dr. Nir Uriel, and impressive results for cytokine reduction using Cytosorb (Dr. Endre Németh). Panel discussions focused on choosing OCS technologies for different donor hearts. Dr. Andreas Zuckermann noted that further trials were needed but current clinical success was strong for both techniques. Dr. Jan Schmitto and Dr. Nir Uriel outlined the benefits of NMP for assessing donor heart viability and suggested MCS could one day replace transplantation, thanks to advances like optimized anticoagulation that reduce bleeding events.
Dr. Kálmán Benke, Associate Professor at the Városmajor Heart and Vascular Center
The roundtable offered a unique and personal insight into the HUNOR – Hungarian to Orbit astronaut mission, with Tibor Kapu and reserve astronaut Gyula Cserényi sharing vivid stories from their training journey and life aboard the International Space Station. The discussion followed the key medical and scientific themes of the HUNOR program, exploring how astronaut selection differs from conventional clinical screening, which physiological parameters define true flight readiness, and how in-flight health is monitored continuously in microgravity. A central message was that Semmelweis University had provided the full medical background and operational health support for the HUNOR program from its inception, including astronaut selection, physical preparation, in-flight medical oversight, and rehabilitation. The astronauts described the physical and psychological stressors of an 18-day mission – from fluid shifts and circadian disruption to cognitive demands – and reflected on the effectiveness of countermeasures designed with the Semmelweis medical team. They detailed the intensive physical training protocol and the challenges of post-flight recovery, particularly rebuilding orthostatic tolerance and muscle strength.
Scientific outputs of the mission, including the TESH multi-sensor cardiovascular monitoring system and the END-SANS ophthalmology project, were also highlighted, demonstrating how Hungarian research contributes to Europe’s growing space-medicine ecosystem. Tibor Kapu and Gyula Cserényi concluded with personal reflections on representing Hungary in space, emphasizing resilience, teamwork, and the long-term scientific legacy the HUNOR program creates for future missions.
Dr. Klaudia Vivien Nagy, Associate Professor at the Városmajor Heart and Vascular Center
Telemonitoring of patients suffering from heart failure has been proven to reduce hospital admissions and mortality, and its use is practically indispensable today. Nevertheless, neither in Hungary nor in other European Union member states has the widespread availability and financing of the system been resolved, as pointed out by Associate Professor Dr. Annamária Kosztin and Dr. Friedrich Köhler. Professor Köhler has led several large-scale randomized trials on remote monitoring and currently heads the telemonitoring center at Charité – Universitätsmedizin Berlin. Remote monitoring allows long-term follow-up of heart failure patients, primarily, but not exclusively, those with implantable cardiac devices. With proper education and health literacy development, patients can become active participants in the telemonitoring process and do more for their own health on a daily basis. Among heart failure patients, those with implantable cardioverter-defibrillators or cardiac resynchronization therapy (CRT) are a particularly vulnerable group. CRT, as presented by Dr. Cecilia Linde, revolutionized the treatment of heart failure more than two decades ago and has shown outstanding results in reducing morbidity and mortality in appropriately selected patients. Dr. Cecilia Linde, President-Elect of the European Society of Cardiology (ESC), has conducted numerous randomized trials in the field of CRT. During therapy, a third electrode is implanted to stimulate the area of the left ventricle that activates last, thereby achieving better pump function. Dr. Cecilia Linde spoke about optimal patient selection and patient responsiveness.
Text: Dr. Annamária Kosztin, Associate Professor and Chief Clinical Physician at the Városmajor Heart and Vascular Center; translation: Dr. Balázs Csizmadia
On the last day of the symposium, the first scientific session in the Basic Medical Science Center explored how multimodality vascular imaging had advanced in recent years and where it was heading. Dr. Robert Edelman (Feinberg School of Medicine, Northwestern University, USA) opened with an overview of cutting-edge MR angiography techniques, showing how faster and clearer scans were bringing radiation-free vascular imaging closer to everyday use. Dr. Hildo Lamb (Leiden University Medical Center, the Netherlands) then demonstrated how MRA had moved beyond anatomy: flow measurements that once belonged to research labs were now becoming part of routine clinical practice.
Dr. Christof Karmonik (Houston Methodist Research Institute, Weill Cornell Medical College, USA) highlighted how detailed vascular MR and artificial intelligence supported pre-procedural planning for endovascular interventions, helping clinicians choose safer and more effective treatment strategies. Dr. Sándor Nardai (Semmelweis University, Hungary) presented new results showing that changes in collateral circulation during patient transfer for thrombectomy could predict outcomes in large-vessel-occlusion stroke, offering valuable insights for acute care pathways. Closing the scientific talks, Dr. Judit Csőre (Semmelweis University, Hungary) reflected on how current vascular imaging practice needed to adapt to emerging clinical demands and technological developments.
The session ended with a lively panel discussion, underscoring a shared vision: future vascular imaging would not only refine diagnosis but also support more personalized, timely, and patient-centered care.
Dr. Judit Csőre, Assistant Lecturer at the Városmajor Heart and Vascular Center
The “Sports Cardiology and Cardiomyopathies” session focused on the complex relationship between athletic cardiac adaptation and cardiomyopathies. The international speakers were Dr. Antonio Pelliccia and Dr. Domenico Corrado from Italy.
Dr. Antonio Pelliccia is Chief of Cardiology at the Institute of Sports Medicine and Science in Rome. His groundbreaking studies on hypertrophic cardiomyopathy and athlete risk assessment have fundamentally shaped how we understand and protect the athletic heart.
Dr. Domenico Corrado was another prominent speaker, an internationally recognized authority in cardiovascular medicine. He is full professor of Cardiovascular Medicine at the Department of Cardiac, Thoracic and Vascular Sciences and Public Health at the University of Padova. His innovative approach to arrhythmogenic and other cardiomyopathies has transformed global practice in sports cardiology, guiding physicians in identifying and protecting individuals at risk of life-threatening arrhythmias, a topic he also elaborated on in his presentation.
The final invited speaker was Dr. Jenő Kamuti – world champion, team world champion, two-time Olympic silver-medalist fencer, surgeon, and one of Hungary’s most respected sports diplomats – who has dedicated his career to promoting fair play and the well-being of athletes.
The major event has already received positive feedback, such as potential international partnership offers. Special thanks go to the main organizers, the colleagues from the Department of Sport Medicine, Dr. Hajnalka Vágó and Dr. Judit Csőre.
Dr. Hajnalka Vágó, Professor at the Városmajor Heart and Vascular Center
Heart failure is currently categorized primarily according to the ejection fraction spectrum. The treatment of patients with reduced (HFrEF) and preserved ejection fraction (HFpEF) may differ in several pharmacological aspects. While in HFrEF the four pillars of therapy clearly have a disease-modifying effect, in HFpEF there have been far fewer proven effective treatments available to date.
Device therapy is also crucial as a supplement to the pharmacological treatment of HFrEF. Cardiac resynchronization therapy (CRT) shows outstanding results in reducing morbidity and mortality in both de novo implantation and upgrade cases. The Budapest CRT upgrade trial, initiated by Dr. Béla Merkely, was the first randomized clinical trial to confirm the efficacy and safety of CRT upgrade in HFrEF patients with pacemakers or ICDs who have a high right ventricular pacing rate. In addition, Dr. Robert Hatala, Professor of Cardiology at the Slovak Medical University in Bratislava and honorary doctor of Semmelweis University, highlighted the importance of treating arrhythmias in patients with heart failure.
Dr. Scott Solomon, Director of the Clinical Trials Outcomes Center at Harvard University and principal investigator of several landmark clinical trials in heart failure, discussed the unique challenges of treating HFpEF. The use of SGLT2 inhibitors has been a breakthrough in this patient group, and based on the latest studies, non-steroidal mineralocorticoid receptor antagonists offer further promise in the treatment of HFpEF patients.
Text: Dr. Annamária Kosztin, Associate Professor and Chief Clinical Physician at the Városmajor Heart and Vascular Center; translation: Dr. Balázs Csizmadia
Dr. Thanila A. Macedo opened the session by exploring contrast-enhanced ultrasound in aortic disease, focusing on its use as an adjunct imaging tool during the transarterial embolization of type 2 endoleaks. She reviewed how the contrast agent improved visualization of endoleaks, perfusion, and graft-vessel interfaces. Her talk framed CEUS as a potential tool to refine decision-making during complex aortic interventions while minimizing contrast load and radiation. This adjunct procedure is likely to increase the clinical success rate of these demanding procedures.
Dr. Csaba Csobay-Novák then turned to physician-modified endografts in aortic repair. He discussed why tailored fenestrations and branches are sometimes necessary when off-the-shelf devices do not match urgent or anatomically challenging cases. The presentation addressed planning, technical steps, and quality-control measures when modifying stent grafts on the back table. Real-world examples helped illustrate when such customized solutions can expand endovascular options for high-risk patients. The presentation highlighted some of the inventions that the Semmelweis Aortic Center had developed in recent years.
Finally, Dr. Jean Paul de Vries focused on prediction of late EVAR failure using CT-based apposition measurements. He emphasized how subtle gaps or poor contact between graft and aortic wall can predispose to endoleaks, migration, or sac enlargement. By systematically quantifying apposition on follow-up CT, clinicians may better stratify risk, decide on closer surveillance, or intervene pre-emptively. His talk positioned advanced imaging analysis as a key component of durable long-term EVAR outcomes.
Dr. Csaba Csobay-Novák, Assistant Professor at the Városmajor Heart and Vascular Center
The session was opened by Dr. Eike Sebastian Debus, Professor at the University Medical Center Hamburg-Eppendorf, Department of Vascular Medicine, former Secretary General of the European Society for Vascular Surgery (ESVS), and recipient of an honorary doctorate from Semmelweis University in 2025. He reviewed the entire spectrum of aortic surgery from the ascending aorta to the bifurcation. He spoke not only about endovascular solutions, but also about how hybrid or even completely open reconstruction remains justified in certain anatomical or clinical situations. He emphasized throughout that the method should be chosen based on the individual patient, rather than sticking to a particular device.
Next, Dr. Péter Banga (Semmelweis University, Városmajor Heart and Vascular Center – Department of Vascular and Endovascular Surgery) showed that, based on the CTA performed for carotid surgery anyway, analysis of the circle of Willis is simple and does not require any new tests – and can show who needs a shunt and who does not. Thus, the decision is based on substantive anatomical information rather than routine.
Dr. Lazar Davidović (University of Belgrade; Clinical Center of Serbia – Vascular and Endovascular Surgery Clinic – one of the world’s largest treatment centers for ruptured AAA) spoke not only about patient care but also about vascular surgery training. In his opinion, high-quality education requires centralization, as otherwise it is not possible to ensure that there is a sufficient number of surgeries and that trainees have uniform experience. Real surgical practice must be preceded by 3D-printed models and cadaver training, thereby reducing the steepness of the learning curve.
Finally, Dr. Fabien Thaveau (University Hospital Strasbourg – French pioneer of robot-assisted vascular surgery) presented the practical side of robotic surgery. He did not characterize it as a miracle weapon, but as a tool that can reduce the number of complications in certain cases, improve manageability in patients in poor general condition, and give both the surgeon and the patient better chances in anatomies where open surgery is particularly difficult, such as in the small pelvis.
Text: Dr. Péter Banga, Assistant Professor at the Városmajor Heart and Vascular Center; translation: Dr. Balázs Csizmadia
The session highlighted how Europe’s emerging space-medicine ecosystem is shaping future human spaceflight. Dr. Serena Pezzilli (Italian Space Agency – ASI) presented the agency’s ongoing cardiovascular research portfolio, emphasizing microgravity-induced vascular remodeling, autonomic dysregulation, and the translational value of astronaut monitoring technologies for terrestrial cardiology. Dr. Alexander Choukèr (LMU Munich) introduced his pioneering immunology studies, detailing stress-induced immune shifts, latent viral reactivation, and the role of neuro-immune mechanisms in human adaptation to extreme environments – insights essential for long-duration missions. Dr. Klaudia Vivien Nagy outlined Semmelweis University’s contributions to the HUNOR program, including the TESH (Telemetry for Space Health) project, which integrates multi-sensor cardiovascular, neuro-vestibular, and metabolic monitoring for real-time astronaut health assessment. She also presented the AIDA AI-assisted point-of-care diagnostics project and the newly established Semmelweis SpaceLab. Collectively, the presentations demonstrated how Hungarian, Italian, and German research efforts converge toward precision space medicine, strengthening Europe’s role in future lunar and Martian exploration.
Dr. Klaudia Vivien Nagy, Associate Professor at the Városmajor Heart and Vascular Center
Dr. Martin Czerny’s live video presentation in the afternoon on the first day of the symposium was a great success.
The definition of the aorta as an independent organ is undoubtedly one of the most significant paradigm shifts of recent years. Dr. Martin Czerny is an energetic multidisciplinary surgeon and researcher whose surgical skills and scientific achievements have attracted interest from multiple professions. After the Semmelweis Symposium, he travelled to a high-profile congress in New York, where he presented his findings urging cooperation between related professions.
The diagnosis and treatment of aortic diseases justify the implementation of multicenter studies, in which our university has already participated (11 joint manuscripts), and we have held promising discussions about future cooperation.
Text: Dr. Zoltán Szeberin, Professor at the Városmajor Heart and Vascular Center; translation: Dr. Balázs Csizmadia
The program, organized by Dr. Nándor Szegedi (Semmelweis University, Városmajor Heart and Vascular Center), focused on the latest clinical studies in the field of electrophysiology. The first section presented left atrial appendage closure and anticoagulation, as well as ablation treatment for atrial fibrillation. This was followed by the “Beat AF” workshop, where world-renowned international professors such as Dr. Pierre Jais, Dr. Daniel Scherr, and Dr. Predrag Stojadinovic gave presentations on electroporation technology.
Text: Dr. Nándor Szegedi, Assistant Professor at the Városmajor Heart and Vascular Center; translation: Dr. Balázs Csizmadia
As part of the symposium, representatives from Central and Eastern European ESC member states were invited to hold a joint session, with the express aim of improving clinical care through cooperation between member states and creating opportunities for further joint studies. The roundtable discussion was attended by renowned professors of cardiology (including the future ESC President, Dr. Cecilia Linde), who presented current and planned clinical studies. Particular attention was paid to the challenges of remote monitoring, especially issues of accessibility and financing. In addition, national registries were presented, and participants discussed their expansion and harmonization at the regional level. During the roundtable discussion, the ongoing Budapest CRT-TAVI prospective randomized trial initiated by Dr. Béla Merkely was outlined, which aims to investigate the effect of CRT in patients who have undergone TAVI implantation and who have persistent left Tawara block and moderately reduced left ventricular function following the procedure.
Text: Dr. Annamária Kosztin, Associate Professor and Chief Clinical Physician at the Városmajor Heart and Vascular Center; translation: Dr. Balázs Csizmadia
The session addressed the rapidly expanding field of right heart imaging, focusing on how contemporary echocardiographic techniques are transforming the assessment of right ventricular (RV) structure and function, as well as the planning and guidance of transcatheter tricuspid valve interventions (TTVI).
Dr. Jörg Hausleiter (Ludwig-Maximilians University of Munich) opened the session with an overview of current transcatheter tricuspid therapies and their imaging requirements. With one of the world’s highest annual volumes of TTVI procedures and participation in several landmark clinical trials, his center has played a defining role in shaping modern tricuspid regurgitation care. He emphasized that the success of TTVI depends heavily on high-quality 3D echocardiography. Detailed anatomical characterization of the tricuspid valve apparatus, accurate leaflet visualization, and understanding of spatial relationships between the valve, right atrium, and right ventricle are essential both for patient selection and intraprocedural guidance. According to Dr. Jörg Hausleiter, 3D imaging has become indispensable for determining feasibility, planning device positioning, and ensuring procedural durability.
The second lecture, delivered by Dr. Attila Kovács (Semmelweis University, Budapest), focused on the evolving methodologies for quantifying RV structure and performance. Dr. Attila Kovács outlined why RV imaging remains one of the most technically demanding areas in echocardiography. He showed how comprehensive 3D volumetric and deformation-derived metrics detect remodeling patterns more sensitively than traditional 2D parameters. He placed particular emphasis on the potential of artificial intelligence in reshaping RV imaging practices. A major theme of his lecture was the urgent need for standardization across centers. Variability in image acquisition, reconstruction, and analysis remains a barrier to broad clinical adoption. Dr. Attila Kovács highlighted ongoing international efforts aimed at establishing unified protocols, quality assurance frameworks, and RV-specific imaging endpoints for future clinical trials.
Dr. Attila Kovács, Assistant Professor at the Városmajor Heart and Vascular Center
Dr. Balázs Csizmadia
Photos by Bálint Barta, Boglárka Zellei – Semmelweis University
Sponsors: