1. Ask for vasoconstriction screening if you are over 60, and warn your elderly family members to do the same.
Lower limb peripheral vascular disease – most often vasoconstriction, the narrowing of blood vessels – can be detected easily and in a timely manner, even when asymptomatic, by feeling the pulse and measuring the so-called ankle-brachial index, a simple and useful test that can be performed by a general practitioner. The result shows the degree of vasoconstriction in the lower limbs compared to the upper limbs. The lower the index, the higher the risk of vasoconstriction.
As age in itself is a risk factor for vasoconstriction, it is recommended for everyone over 60 to ask for this screening test, as well as a laboratory test, to rule out diabetes or a disease with high blood fat levels.
If you smoke, are overweight, or have been diagnosed with diabetes or a disease with elevated blood fat levels, regular check-ups are essential because the risk of vasoconstriction increases significantly, emphasizes Dr. Péter Sótonyi, Head of the Department of Vascular and Endovascular Surgery at the Városmajor Heart and Vascular Center.
If you have a history of vasoconstriction affecting the heart, coronary arteries, or brain vessels, you should get checked for other narrowing in the vascular system, he advises.
2. Take the loss of walking distance and non-healing wounds seriously.
 Limb-threatening vasoconstriction is most commonly seen in smokers and diabetics. In severe cases of vasoconstriction, a clear warning sign is exercise-induced crampy, muscle-fever-like pain in the lower limbs, mostly in the calf, but also in the thighs and buttocks. It can be so bad that it makes the patient stop for a few minutes, a symptom known as intermittent claudication. A gradually shorter walking distance is an important warning sign. If you have the slightest exercise-induced complaint, it’s imperative to go for a check-up, Dr. Péter Sótonyi points out, adding that a non-healing wound and toe gangrene are similarly serious symptoms. The primary aim is to save the limb, but it is important to seek medical advice in good time because even if amputation cannot be avoided, it makes a difference to the quality of life whether only a toe or an entire leg has to be cut off, he explains.
Limb-threatening vasoconstriction is most commonly seen in smokers and diabetics. In severe cases of vasoconstriction, a clear warning sign is exercise-induced crampy, muscle-fever-like pain in the lower limbs, mostly in the calf, but also in the thighs and buttocks. It can be so bad that it makes the patient stop for a few minutes, a symptom known as intermittent claudication. A gradually shorter walking distance is an important warning sign. If you have the slightest exercise-induced complaint, it’s imperative to go for a check-up, Dr. Péter Sótonyi points out, adding that a non-healing wound and toe gangrene are similarly serious symptoms. The primary aim is to save the limb, but it is important to seek medical advice in good time because even if amputation cannot be avoided, it makes a difference to the quality of life whether only a toe or an entire leg has to be cut off, he explains.
The most common vascular diseases
There are almost 100,000 kilometers of blood vessels in our bodies, and they can be divided into two large groups: arteries (carrying blood away from the heart) and veins (carrying blood towards the heart). The most common arterial diseases include vasodilatation (widening of blood vessels) and vasoconstriction (narrowing of blood vessels), while the most common venous diseases are varicose veins, and the most serious is deep vein thrombosis, which is a blood clot that forms in the lower limb, blocking the free flow of blood. Pulmonary embolism caused by a blood clot breaking off can be a life-threatening complication. Blood clots can also develop in the arteries, which is the most common cause of heart attack and stroke.
3. Get your varicose veins checked if you have heavy legs or other complaints.
Varicose veins are conditions affecting the veins. Although the prevalence increases with age, those who are susceptible to it can develop symptoms at a younger age. The milder form of varicose veins is usually just a cosmetic ailment. It can cause a problem when the vein dilates due to the insufficient functioning of the valves in the varicose vein, resulting in poor circulation in the affected limb. This is when the first symptoms start to appear, such as heavy legs, limb strain, leg cramps (especially at night), and restless leg syndrome. In this case, especially if you have a family history of varicose veins, it is always worth showing your veins to your GP, who will be able to assess whether you need to see a specialist.
Deterioration is indicated by skin changes such as discoloration, itchy rashes, and large bulging veins all over the body; the final stage is when a venous ulcer develops, which requires treatment. If you notice any of the above symptoms, it is worth seeking medical advice even if you do not have visible varicose veins, as there are often no early signs of chronic insufficiency of deeper veins. The latter can also include swelling in the ankles and feet, leg cramps at night, and the most serious form is venous leg ulcers, which are wounds that take weeks to heal, and can also lead to deep vein thrombosis if a blood clot develops in a deep vein. The risk of developing deep vein thrombosis may increase if you have a family history of thromboses, but it can also be increased by certain medications (such as contraceptives), prolonged immobility of the leg (on long flights, car journeys, or when being bedridden), being overweight, and smoking.
In the vast majority of cases, varicose veins only require surgical intervention for esthetic purposes. In such cases, only the smaller, lateral veins can be operated on, and the so-called superficial main vein can only be removed if a venous insufficiency is confirmed by an ultrasound scan. The worst for varicose patients is prolonged standing or sitting, which increases the risk of thrombosis and other complications. If you have a sedentary job, slightly elevate your legs, and if you have a standing job, move your muscles from time to time (e.g., by standing on tiptoe). These may help with mild complaints. Treatment options for venous insufficiency include taking antioxidant flavonoids to strengthen the vascular wall and wearing compression stockings to improve vein circulation. Only in severe cases should surgery or the use of special medication (such as blood thinners) be considered.
4. Hydrate more and quit smoking: Although vascular diseases tend to run in families, there are things you can do to prevent them.
 The first and foremost step we can take to avoid venous and arterial diseases is to quit smoking completely, emphasizes Dr. Péter Sótonyi. Studies have shown that the risk of developing vascular disease significantly decreases after just five smoke-free years, and after ten years, the risk is comparable to the general population. In addition, achieving optimal body weight, exercising, and following a proper diet rich in vegetables but low in carbohydrates, fats, and salt are of particular importance. Adequate fluid intake is paramount in vascular disease, as in people at risk, low fluid intake and inactivity can contribute to developing blood clots, which may lead to thrombosis.
The first and foremost step we can take to avoid venous and arterial diseases is to quit smoking completely, emphasizes Dr. Péter Sótonyi. Studies have shown that the risk of developing vascular disease significantly decreases after just five smoke-free years, and after ten years, the risk is comparable to the general population. In addition, achieving optimal body weight, exercising, and following a proper diet rich in vegetables but low in carbohydrates, fats, and salt are of particular importance. Adequate fluid intake is paramount in vascular disease, as in people at risk, low fluid intake and inactivity can contribute to developing blood clots, which may lead to thrombosis.
Lifestyle change is a long-term investment where the returns are measured in life years. Although many people think of vascular disease as affecting the elderly, the lifestyle problems that usually lead to vascular disease start at a younger age. – Dr. Péter Sótonyi
Familial clustering is also a decisive factor, so if you have a family history of vascular disease, be sure to inform your doctor, as this will require even more frequent monitoring and maintaining lower blood fat and blood sugar levels. Patients at high risk may require continuous medication (such as blood sugar and blood fat-lowering drugs, aspirin derivatives).
5. Take some simple tests to predict the possible risk of hazardous acute vascular diseases.
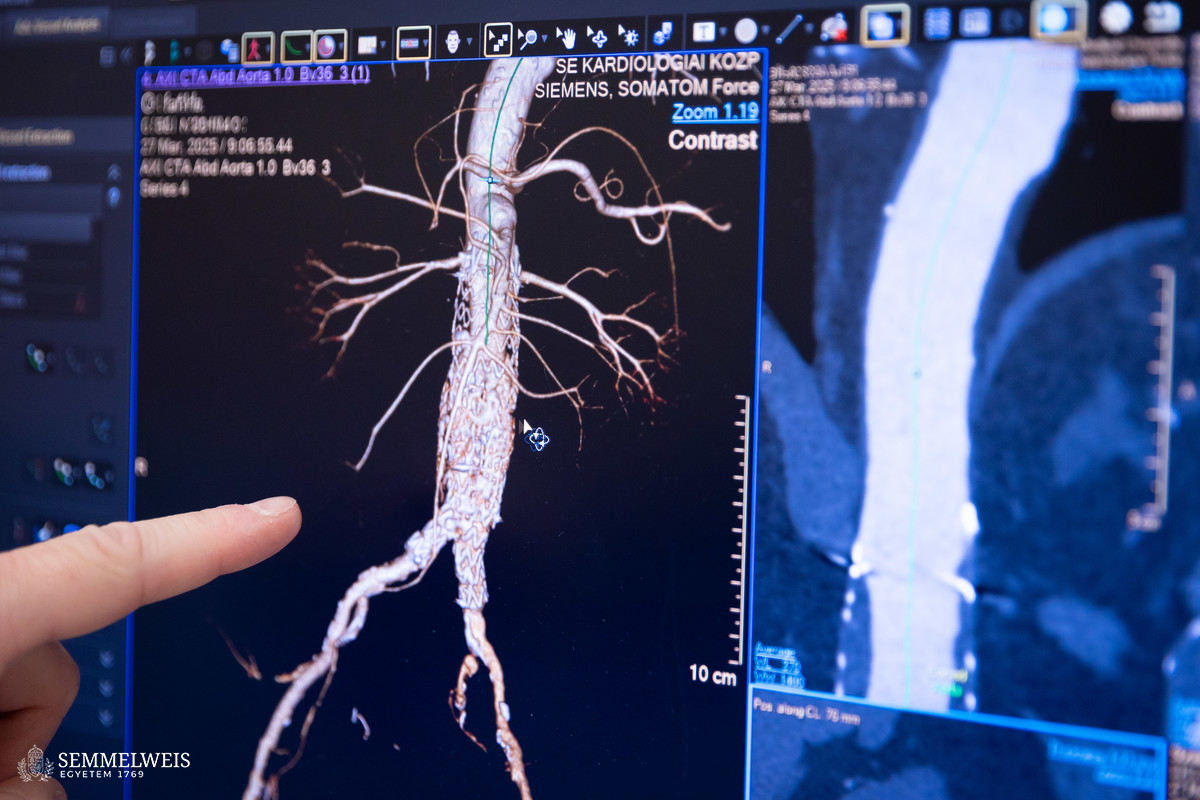
Vasodilatation, an arterial disease that most often affects the main arteries in the abdomen and chest (aorta), usually produces no or only nonspecific symptoms (such as back pain or pulse in the stomach).
That is why it is recommended for patients in the most vulnerable group, i.e., smoking men over 65, to have an abdominal ultrasound scan, because it can detect a dilatation in the abdominal aorta, the so-called aneurysm, which accounts for two-thirds of cases, Dr. Péter Sótonyi points out.
If its diameter exceeds 5 centimeters for women and 5.5 for men, surgery is required, he adds. Early detection is vital because if the dilated vessel has already ruptured and surgery is only performed afterwards, the risk of mortality is ten times higher. Smoking is an even stronger factor in developing aortic aneurysms compared to aortic stenosis, as someone who has this condition and smokes is almost seven and a half times more likely to develop and grow an aneurysm, and thus to suffer a life-threatening rupture of the vessel wall.
In acute (sudden onset) circulatory failure in the limbs, most commonly caused by embolism from the heart or localized blood clots in the limb, the time window for the vascular specialist is very short, so rapid recognition is crucial. Signs of this include the sudden onset of pain, the absence of pulse, and a cold limb. In more severe cases, loss of sensation and mobility occur. In such cases, the patient should be referred to specialist care as soon as possible so that the limb can be saved.
Stroke can also be an acute, life-threatening condition, which in many cases is caused by a narrowing of the carotid artery, detectable by carotid ultrasound.
Warning signs may include temporary loss of vision, numbness in the opposite hand, hand weakness, or one-sided muscle weakness. If we start treating carotid artery stenosis early enough (by lowering blood lipid levels and applying anticoagulant therapy), we can slow down the deterioration of the condition and the risk of stroke, the head of the department points out.
Pálma Dobozi
Translation: Judit Szabados-Dőtsch
Photos by Boglárka Zellei – Semmelweis University; iStock (varicose vein illustrations)