While previous editions of the event gave an overview of the state of transplantation, the 2024 symposium focused on a particular segment of the field, machine perfusion.
This technique is used for transplanting organs from deceased donors. Its significance lies in the possibility of circulating specific fluids to the abdominal or thoracic organs to be transplanted (kidneys, liver, heart, and lungs), thereby nourishing and simultaneously oxygenating the cells, as opposed to the cold storage and organ transport routinely used until now. This helps to reduce the degree of cell damage that occurs during conventional cold storage and thus prevent premature dysfunction of the transplanted organ, which can pose a serious risk to the patient.
 In his welcome address, Director Dr. Attila Szijártó highlighted that since the establishment of the Department of Surgery, Transplantation and Gastroenterology (STéG), Transplant Today has become a flagship event series of the institution. Not long ago, Hungary has celebrated the 50th anniversary of its kidney transplantation program, and will soon reach the 30-year milestone of the institutionalized liver transplantation program, he added. Dr. Attila Szijártó considered the recent split liver transplant performed at the clinic a remarkable technical achievement, which involved dividing the organ to be transplanted into two portions, one for a small child and one for an adult. Following this, the introduction of machine perfusion would be a long-awaited addition to the institution’s portfolio.
In his welcome address, Director Dr. Attila Szijártó highlighted that since the establishment of the Department of Surgery, Transplantation and Gastroenterology (STéG), Transplant Today has become a flagship event series of the institution. Not long ago, Hungary has celebrated the 50th anniversary of its kidney transplantation program, and will soon reach the 30-year milestone of the institutionalized liver transplantation program, he added. Dr. Attila Szijártó considered the recent split liver transplant performed at the clinic a remarkable technical achievement, which involved dividing the organ to be transplanted into two portions, one for a small child and one for an adult. Following this, the introduction of machine perfusion would be a long-awaited addition to the institution’s portfolio.
In his keynote presentation, Dr. Sándor Mihály, Head of Transplantation Directorate at the Hungarian National Blood Transfusion Service (OVSZ) and Chair of the European Donation and Transplantation Coordination Organization (EDTCO) introduced the national machine perfusion program plan of Hungary. He started by making it clear that despite its costs, the development of national organ donation and transplantation programs is rather to be regarded as an investment. These programs aim at maximizing the health benefits for patients by both increasing the number of life years gained and improving the quality of life. With 131 donations in 2023 and an average organ donor securing 30.8 additional life-years, a total of 4,035 life-years were made possible last year. This happens against a backdrop of chronic diseases, which impose a substantial burden on healthcare systems. Although there is an increasing demand for organ replacement therapies, artificial organ support is restricted to certain instances, as it is only available in a large scale for kidney failure patients in the form of dialysis.
 Dr. Sándor Mihály cited the WHO, which called on governments and healthcare professionals to pursue self-sufficiency in transplantation by using resources from within their own population. Self-sufficiency entails a combination of strategies targeted at decreasing the burden of diseases treatable through transplantation and at maximizing the availability of organs for transplantation, with priority given to donation from the deceased. It is countries with well-established donation programs that have achieved the highest transplantation rates and best access of their patients to transplant therapy, he highlighted.
Dr. Sándor Mihály cited the WHO, which called on governments and healthcare professionals to pursue self-sufficiency in transplantation by using resources from within their own population. Self-sufficiency entails a combination of strategies targeted at decreasing the burden of diseases treatable through transplantation and at maximizing the availability of organs for transplantation, with priority given to donation from the deceased. It is countries with well-established donation programs that have achieved the highest transplantation rates and best access of their patients to transplant therapy, he highlighted.
Moreover, a 2009 cost-effectiveness study for end-stage kidney failure patients in the United Kingdom has shown that the annual savings of transplantation compared to dialysis amount to 84 percent. Further European statistics and literature suggest that transplantation is a crucial investment for the future resilience of healthcare systems, with certain questions of reimbursement still open in the majority of countries involved.
As Dr. Sándor Mihály outlined, the Hungarian machine perfusion initiative dates back to 2018, when the first proposal and recommendation for heart machine perfusion procedure was drafted, followed by the proposal for kidney program in 2021. As a result, the purchase of machine perfusion devices was scheduled within an EU-funded project in 2021.
The current budget plan for 2025 includes the acquisition of one heart, one lung, one liver and two kidney machine perfusion devices through public procurement, with additional public procurement procedures for consumables ensuring five heart, five lung, 10 to 15 liver, and 50 kidney transplantations annually.
In general, the introduction of machine perfusion is justified by the increase in the number of possible transplants, as it allows for longer cold ischemia time, i.e. longer preservability, organ transport from a longer distance, and acceptance of extended criteria donor organs, Dr. Sándor Mihály emphasized. Moreover, it ensures quality enhancement, since machine perfusion not only optimizes the timing of transplantation, but also improves the quality of organs and thus results in longer graft and patient survival. This technique can also be used to model the functioning of organs after a possible transplantation, and can be used for instrumental testing or quality improvement interventions. With a national machine perfusion program, equal access to centers and patients can be safeguarded.
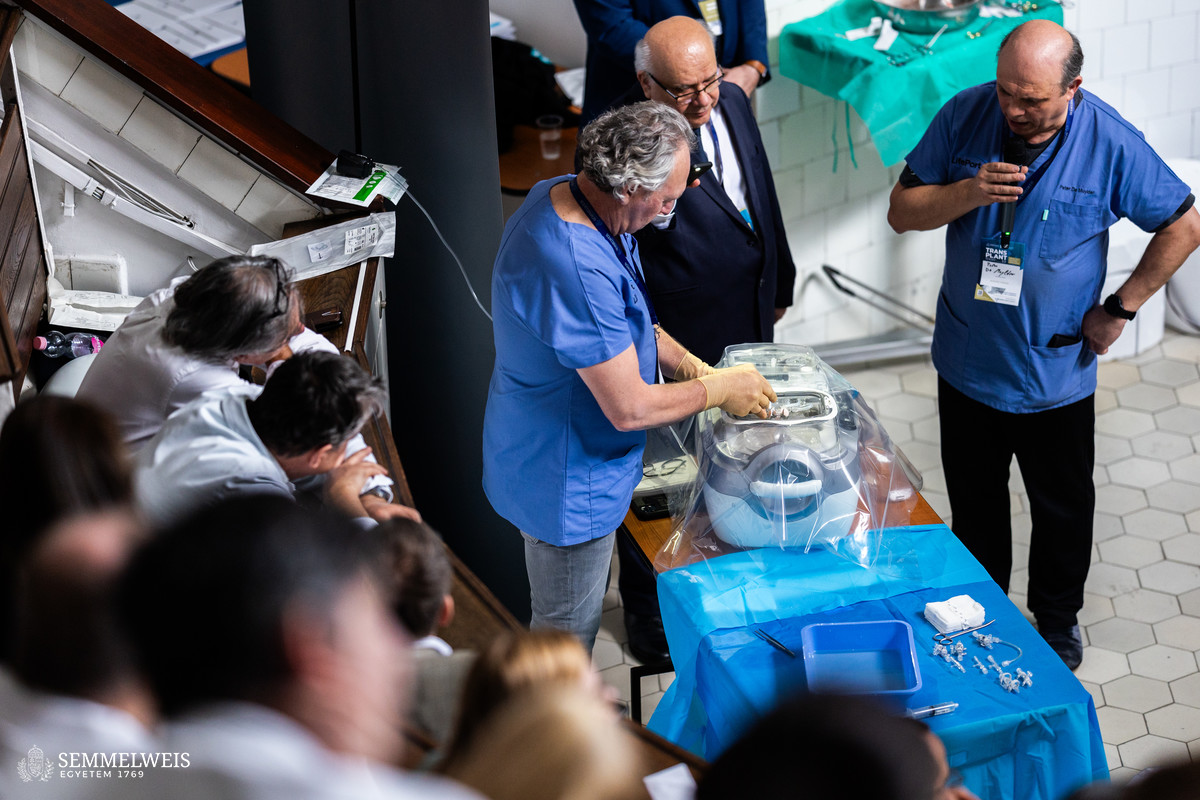
In the follow-up session, American, Swedish, and Italian companies at the forefront of transplantation machine perfusion device manufacturers presented their products. The live demonstration included a perfusion of previously removed porcine kidneys, offering attendees a hands-on experience of the technology.
The devices presented by the companies are suitable for hypothermic or normothermic perfusion of the kidneys, liver, heart and lungs, but a machine perfusion unit was also presented that allows the treatment of different organs depending on the program.
Machine perfusion can also be used for selected liver surgeries. Thus, for instance, if the removal of a liver tumor would pose a high risk, it is possible to temporarily remove the liver, which can then be safely operated on the preparation table (ex situ) or even during machine perfusion without patient blood loss. After removal of the diseased parts, the liver can be autotransplanted after a few hours of perfusion and restored to its original position. This autotransplantation, already performed worldwide on numerous occasions, has saved the lives of dozens of patients by removing tumors previously presumed inoperable.
The live demonstration gave the professional attendees the opportunity to get acquainted with the machines that will soon be acquired and to learn about their features. This will also help to optimize the composition of the domestic machinery fleet in line with the needs of the sector.
In the closing session of the symposium, STéG faculty members, Associate Professor Dr. László Piros, Associate Professor Dr. Tamás Benkő and Assistant Professor Dr. Gergely Huszty conducted a panel discussion on machine perfusion of the kidney and liver, based on German and Italian examples. Dr. István Hartyánszky, President of the Hungarian Transplant Society, and Dr. Balázs Gieszer, Clinician at the Department of Thorax Surgery reviewed this innovative procedure from the perspective of heart and lungs transplantations, respectively, in preparation for its introduction in Hungary.
Judit Szabados-Dőtsch
Photo: Bálint Barta, Boglárka Zellei – Semmelweis University