Basic sports cardiology examinations
Basic examinations include acquiring an accurate and detailed patient history with special regards to inherited (cardiac) diseases and sudden cardiac death in family history. We perform a physical examination, 12-lead ECG and laboratory tests on a regular basis.
Exercise tests
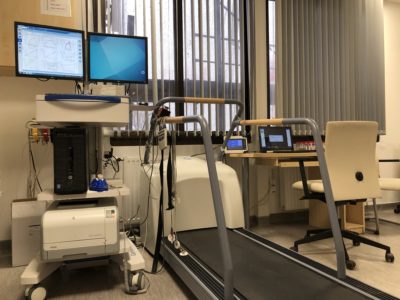 At our outpatient clinic we perform cardiopulmonary exercise testing (CPET) in high volume on treadmill and cycle ergometer. With the help of CPET we are able to monitor and follow the athletes’ maximal exercise capacity and are able to give recommendations to the trainer on the optimization of the training programme. In addition, symptoms that occur only during physical activity, such as arrhythmias may be identified during exercise testing. It is a complex examination modality: we are able to gather data on the individuals’ cardiopulmonary system’s state as well as metabolic fitness by measuring fingertip capillary lactate levels.
At our outpatient clinic we perform cardiopulmonary exercise testing (CPET) in high volume on treadmill and cycle ergometer. With the help of CPET we are able to monitor and follow the athletes’ maximal exercise capacity and are able to give recommendations to the trainer on the optimization of the training programme. In addition, symptoms that occur only during physical activity, such as arrhythmias may be identified during exercise testing. It is a complex examination modality: we are able to gather data on the individuals’ cardiopulmonary system’s state as well as metabolic fitness by measuring fingertip capillary lactate levels.
Laboratory tests
In case of various diseases, symptoms and family history blood tests are fundamental in the diagnostic work-up in sports cardiology as well as other fields of medicine. Above the age of 35, in (master) athletes we perform a yearly blood test consisting of blood count, liver and kidney function and cholesterol measurements, however we often perform extended laboratory testing in young athletes too.
Regardless of age we can optimize athletes’ performance by measuring iron and vitamin D levels and apply the necessary dietary and medical modifications.
It is important to remark that there are no universally accepted, available normal values for (elite) athletes regarding several lab parameters. Therefore it is always important to consult an internist/cardiologist/sports’ medicine specialist with the results – the evaluation should always be individualized.
Echocardiography
 Due to the availability, noninvasiveness and the ability to provide abundant information on cardiac function and morphology echocardiography is regarded as a basic diagnostic tool in cardiology thus in sports cardiology too.
Due to the availability, noninvasiveness and the ability to provide abundant information on cardiac function and morphology echocardiography is regarded as a basic diagnostic tool in cardiology thus in sports cardiology too.
The method involves a transducer that contains piezoelectric crystals that emit ultrasound. By detecting and transforming these signals we are able to create 2D and 3D images to display the heart’s various aspects.
Regular (vigorous) physical activity causes various changes in cardiac function and morphology. Athletes’ heart can be characterized by elevated left and right ventricular muscle mass and elevated volume of the different chambers of the heart.
By the help of echocardiography we are able to identify different types of congenital heart disease and valvular diseases as well.
In those cases when echocardiography is not conclusive performing cardiac MRI is recommended.
Cardiac CT, invasive coronarography
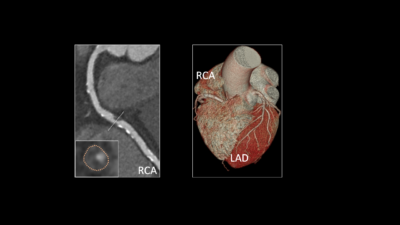 The burden caused by coronary vessel disease in athletes is mainly acknowledged in the master age group (above 35). In 80% of sudden cardiac death cases in the aforementioned age group malignant ventricular arrhythmias caused by myocardial infarction is the responsible underlying condition.
The burden caused by coronary vessel disease in athletes is mainly acknowledged in the master age group (above 35). In 80% of sudden cardiac death cases in the aforementioned age group malignant ventricular arrhythmias caused by myocardial infarction is the responsible underlying condition.
In the vast majority of cases chest pain (angina) occuring at rest or during exercise indicates further diagnostic work-up other than basic examination methods. The examining doctor may suggest performing a noninvasive or an invasive coronarography to exclude or confirm coronary artery disease.
 In general, in symptomatic, stable patients that are considered to have low or moderate risk for coronary artery disease are advised to go through coronary CT angiogram (CTA).
In general, in symptomatic, stable patients that are considered to have low or moderate risk for coronary artery disease are advised to go through coronary CT angiogram (CTA).
Rarely, young athletes may unfortunately suffer sudden cardiac death due to coronary origin anomaly.
It is important to highlight that CTA and invasive coronary angiogram should only be utilised with established indication as they both utilize ionizing radiation (x-ray) and contrast agent. In case of positive results there may be need for further test such as stress echocardiography or stress MRI.
Heart MR
 Cardiac magnetic resonance examinations are considered to be one of the most innovative noninvasive imaging techniques. It is the gold standard method to measure cardiac volumes and function. We are able to gather information on the heart in the desired depth and plane without using ionizing radiation.
Cardiac magnetic resonance examinations are considered to be one of the most innovative noninvasive imaging techniques. It is the gold standard method to measure cardiac volumes and function. We are able to gather information on the heart in the desired depth and plane without using ionizing radiation.
In the MRI room there is a strong magnetic field present. Other than that radiofrequency excitation is necessary to acquire the images.
In the suspicion of myocarditis, ischaemia and structural heart diseases, with the help of cardiac MRI we can obtain myocardial tissue information by using contrast media containing Gadolinium (Gd). On the other hand, novel techniques are being developed to diagnose the aforementioned conditions without the necessity of using contrast agent.
In the athlete population we usually perform cardiac MRI in the case of a suspected structural heart disease (e.g. hypertrophic cardiomyopathy, arrhythmogenic cardiomyopathy, dilated cardiomyopathy), myocarditis, positive family history for inherited cardiac disease or congenital diseases.
Sometimes it is challenging to differentiate between a physiologically adapted athletes’ heart and a pathologic condition. Even a physiologically adapted heart can share some similarities with a diseased heart and most of the cases cardiac MRI is able to differentiate between the two.
Holter (24-hour) ECG, ABPM
Several types cardiac arrhythmias are not present at the time of registration of a resting 12-lead ECG. In these cases a 24 hour (or longer) Holter ECG monitoring might be necessary to identify the arrhythmia type and/or its burden on the patient. The Holter device is set up at our outpatient clinic and consists of a small central device and electrodes.
If irregular heartbeats are experienced during rest or exercise, also if there is suspicion of too fast or too slow heart rate Holter ECG monitoring might be able to reveal the type of arrhythmia.
ABPM (ambulatory blood pressure measurement) is utilized to establish or exclude the diagnosis of hypertension. The device consists of a central unit and a cuff and is placed at our outpatient clinic. The examination usually lasts for 24 hours.
In spite of the cardiovascular risk reducing effect of regular physical activity athletes can also develop a hypertensive condition. Similarly to non-athletes the risk gradually increases as an individual gets older. Proper management of hypertension by diet, lifestyle modification, pharmacological therapy is essential to ensure safe sport activity and prevention of possible future cardiovascular events. If necessary, the selection of the most suitable pharmacological therapy is essential to ensure proper blood pressure lowering effect while not cutting back performance and also to avoid doping fault.
Electrophysiology (EP)
Electrophysiology is the subspecialty in cardiology that focuses on the treatment of arrhythmias. Involving an expert is often necessary when having an athlete diagnosed with a cardiac arrhythmia that requires an invasive approach. The conditions concerning the athlete population can be treated and/or cured by catheter ablation techniques with expressly good efficacy.