Projects
Research Group Leader:
Dr. Mahmoud Al-Khrasani, Associate Professor (Google Scholar)
Our research team at the Department of Pharmacology and Pharmacotherapy continues the Institute’s longstanding tradition of behavioral pharmacological research, focusing on pain and pain management. While pain relief may appear to be a solved issue at first glance, existing medications can be insufficient in certain cases—such as neuropathic pain—and all currently available analgesics have serious side effects. Although behavioral pharmacology might seem outdated, it remains indispensable in psychopharmacology. A recurring challenge in psychopharmacological drug development is that compounds that appear promising and effective in animal models frequently fail during clinical trials, suggesting that current animal models offer limited translational value.
Pain Research Methodology
In our pain research, we primarily use in vivo pain models, supplemented as needed with ex vivo (isolated organ) and in vitro (binding assays, immunohistochemistry, PCR, Western blot, etc.) techniques. These latter methods are partly conducted in collaboration with both domestic and international partners (e.g., the Hungarian Academy of Sciences; Charité – Universitätsmedizin Berlin).
In Vivo Pain Models
Currently, there is no satisfactory way to model pain in vitro, making in vivo animal experimentation indispensable for investigating analgesic substances and procedures.
- Acute Nociceptive Tests:
- Tail-flick test
- Hot-plate test (traditional and ramped-temperature variants)
- Inflammatory Models:
- Acute: Formalin test, acetic acid–induced writhing test (duration: 1 hour)
- Subacute: Carrageenan-induced inflammatory hyperalgesia (duration: 3–5 hours)
- Subchronic: Complete Freund’s Adjuvant (CFA)–induced hyperalgesia (duration: 3–7 days)
- Neuropathic Models:
- Seltzer’s partial ligation of the sciatic nerve, resulting in mononeuropathy (duration: 1–3 weeks)
- Diabetes-induced polyneuropathy (duration: 6–12 weeks)
Cognitive Tests
- 5-Choice Serial Reaction Time Task – attention and impulsivity
- Morris Water Maze – spatial memory
- Barnes Maze – spatial memory
- Novel Place Recognition Test – spatial memory
- Spontaneous Alternation – short-term spatial memory
- Cooperative Task in a Skinner Box – social cognition
- Cooperation on a Seesaw – social cognition
- Rescue Box Test – social cognition
- Novel Object Recognition Test – recognition memory
- Fear Conditioning – fear memory
- Passive Avoidance – fear memory
- Shuttle Box – fear memory
- Pot-Jumping – motor learning
- Automated Movement Pattern Analysis in an Open Field – locomotor activity
- Elevated Plus Maze – anxiety
- Conditioned Place Preference – testing substances with addictive or aversive potential
- General, Hypo-, and Hyper-locomotor Activity measurements
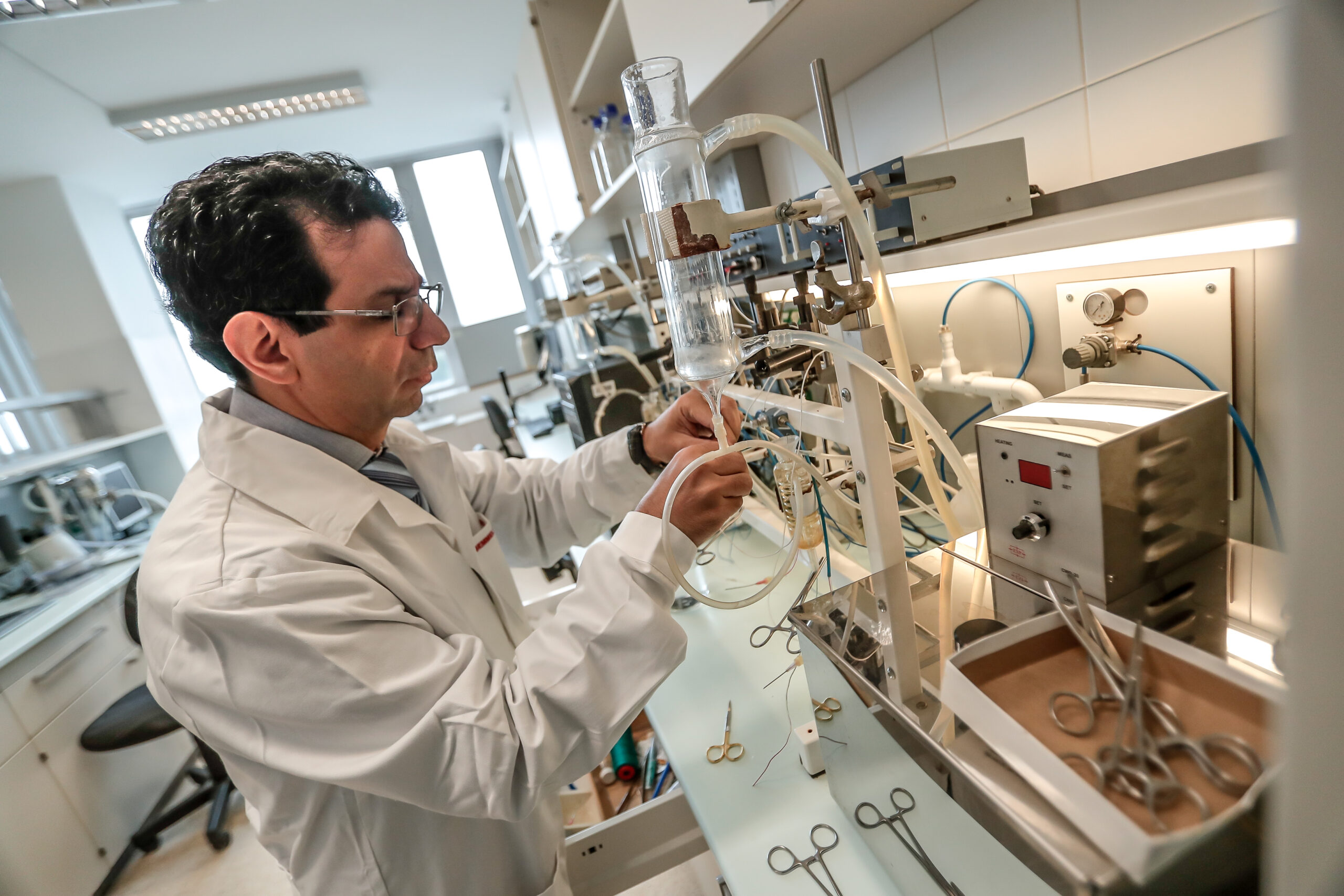
Ex Vivo (Isolated Organ) Measurements
One classic ex vivo method for screening opioid analgesics involves experiments on isolated organs. Three tissue types are commonly used:
- Mouse vas deferens (containing δ and μ opioid receptors)
- Rat vas deferens (expressing few μ receptors; only highly intrinsic activity ligands are effective)
- Guinea pig ileum longitudinal strip (κ and μ receptors)
This approach enables cost-effective screening of new (putative) opioid ligands and can also be used to study drug interactions or to model tolerance.
In Vitro Assays
From animals assessed in various pain models, we isolate tissues after the in vivo measurements to determine receptor density and transmitter levels. We use both quantitative methods (capillary electrophoresis, PCR, Western blot) and semi-quantitative techniques (RNAScope, immunohistochemistry). Depending on the specific research focus, we concentrate primarily on central nervous system regions that are critical for pain transmission.
Ongoing Research Projects
1. Glycine Transporter Inhibitors in Pain and Opioid Analgesic Tolerance
Glycine plays a dual role in the central nervous system: it acts as an inhibitory neurotransmitter via its own receptor and also serves as an NMDA receptor co-agonist, thus regulating excitatory neurotransmission. Excessive NMDA receptor activity is a key factor in the development of neuropathic pain and opioid analgesic tolerance. Although NMDA receptor antagonists are effective against neuropathic pain and help reduce opioid tolerance, their side effects (e.g., cognitive dysfunction) limit clinical use. Consequently, alternative strategies for regulating NMDA receptor function are needed. One possibility is to modulate glycine levels by inhibiting its transporters, an approach that may initially boost, then secondarily decrease, receptor activity through desensitization.
Our goal is to investigate how glycine transporter inhibitors affect neuropathic pain and opioid analgesic tolerance. Thus far, our results are promising: in neuropathic pain models, these inhibitors reduced allodynia and mitigated the development of morphine tolerance during chronic treatment.
2. The Renin–Angiotensin System (RAS) in Pain and Opioid Analgesic Tolerance
A growing body of evidence suggests that the renin–angiotensin system (RAS) modulates pain at multiple levels (e.g., dorsal root ganglia, spinal cord). However, the precise mechanisms remain to be clarified. Our group previously demonstrated that antagonists of the angiotensin II type 1 receptor (AT1 receptor)—telmisartan and losartan—can alleviate mononeuropathic pain. We also observed that a subanalgesic dose of telmisartan restored morphine efficacy in neuropathic rats and reduced morphine-induced analgesic tolerance.
We aim to use immunohistochemistry and Western blot to elucidate the mechanism through which AT1 receptor antagonists modulate neuropathic pain and opioid analgesic tolerance. We also plan to investigate their effects on fentanyl-induced analgesic tolerance.
3. Tolperisone for Neuropathic Pain and Opioid Analgesic Tolerance
Tolperisone is a centrally acting muscle relaxant developed in Hungary but relatively lesser-known worldwide. Uniquely among similar drugs, tolperisone does not produce sedative side effects. Although its precise mechanism is not fully understood, it is believed to predominantly act via sodium channel blockade. In recent years, our team, in collaboration with Meditop Zrt., has explored repurposing tolperisone for neuropathic pain. Based on our published animal data, tolperisone shows significant potential both as a standalone therapy and in combination with other neuropathic pain agents.
4. Kratom: A New Generation of Analgesics
(Details forthcoming.)
Developing a Clinically Relevant, Translational Cognitive Experimental Model
Our objective is to create a complex cognitive experimental framework that surpasses currently available methods in predictive value and accuracy when identifying clinically effective cognitive-enhancing mechanisms.
Learning capacity and memory are impaired in various neurological and psychiatric disorders (e.g., Alzheimer’s disease, schizophrenia, autism). Current therapeutic options provide only limited benefit in alleviating these symptoms, underscoring the need for effective cognitive enhancers.
Despite ongoing basic research discovering new cognitive-enhancing mechanisms, the clinical development of such agents has faced near-total attrition over the past decade. This translational gap could be due to inadequate selection of molecular targets and the low predictive value of animal models.
Potential therapeutic targets identified by basic research must be rigorously validated in appropriate animal models to ensure their suitability for pharmaceutical development. However, many existing models yield large numbers of false positives—compounds that appear promising preclinically but show no therapeutic benefit in humans. This shortcoming likely arises from the simplicity of conventional approaches: for instance, impairing a single elementary memory function (e.g., passive avoidance or novel object recognition) with a single dose of a pharmacological agent (e.g., scopolamine) may not accurately reflect the robust cognitive deficits seen in clinical populations. More complex paradigms with greater translational value are needed.
In this project, we train rats and mice in multiple learning paradigms (see the list of methods above). Each task models a distinct human cognitive function typically assessed in clinical practice. Some animals undergo training in several tasks, creating a broad-based “knowledgeable” population.
To test potential cognitive enhancers, animals’ performance is first reduced. The method of impairment is pivotal for modeling the cognitive deficits of a specific disorder. Learning can be impaired pharmacologically (e.g., scopolamine), genetically, by environmental stress, or by selecting inherently poor-learning or aged animals. By applying such interventions, we obtain a “patient population” of animals with significant cognitive deficits.
Next, we evaluate putative enhancers across a wide range of cognitive functions in these “patient” animals, employing a methodology analogous to clinical trials: double-blind, placebo-controlled, randomized experiments with (sub)chronic drug administration.
Mechanistic Studies of “Enhancer” Compounds Acting at TAAR Receptors
In the early 1960s, Knoll and colleagues developed (-)-deprenyl (selegiline), the first selective monoamine oxidase B (MAO-B) inhibitor, which is widely used in the treatment of Parkinson’s disease, major depression, and as an adjunct therapy in Alzheimer’s disease. Knoll observed that at low doses (-)-deprenyl enhances learning and memory and slows brain aging. He termed this phenomenon the “enhancer effect” (Knoll, 2003). This effect can be induced by (-)-deprenyl—primarily by increasing catecholaminergic tone—or by R-(-)-1-(benzofuran-2yl)-2-propylaminopentane [(-)-BPAP], which boosts both catecholaminergic and serotonergic activity in the CNS.
Enhancer compounds augment stimulus-induced biogenic amine (norepinephrine, dopamine, serotonin) release at very low concentrations, likely through activation of trace amine-associated receptors (TAAR) and by increasing the function of the vesicular monoamine transporter 2 (VMAT2). Our research aims to define the detailed mechanism of this enhancer effect. TAAR receptors may represent a novel therapeutic target for managing neurodegenerative disorders.
In upcoming experiments, we will investigate how different compounds (e.g., TAAR agonists, TAAR antagonists, and both endogenous and synthetic enhancer substances) influence cognitive functions in various behavioral pharmacological tests. Alongside evaluating cognition-enhancing potential, we are also examining whether TAAR-targeting compounds could have analgesic properties, parallel to our ongoing pain-related studies.
Members
Group leader:
Mahmoud Al-Khrasani, (PharmD, PhD, Dr.Habil) Associate Professor
Researcher:
István Gyertyán, (PhD) Senior Researcher
Ildikó Miklya, (PharmD, PhD) Associate Professor
Pál Riba, (MD, PhD) Associate Professor
Kornél Király, (MD, PhD) Associate Professor
Alíz Ernyey, (PhD) University Assistant Professor
Scientific advisors:
Zsuzsanna Fürst, (MD, DSc) Emeritus Professor
László Gábor Hársing, (MD, DSc) Scientific Advisor
Júlia Timár, (MD, PhD) Associate Professor
PhD students:
Nariman Gomaa Essmat Mohamed Aldeltawab, (MSc)
Sarah Abood Kadim Alkafage, (MSc)
Anna Galambos, (MSc)
Bence Tamás Varga, (MSc)
Imre Boldizsár, (MD)
Yashar Chalabiani, (PharmD)
Sandra Marouf, (MSc)