|
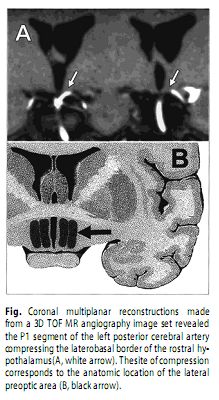
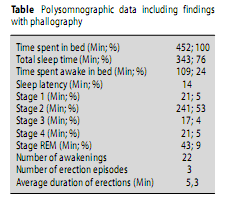
A. Szücs,M.D., J. Janszky,M.D., Ph. D., P. Barsi,M.D., Z. Clemens, G.Migléczi, M.D., Received: 15 July 2001 Sirs: Erections are normal phenomena during sleep [4–6, 9]. Sleep-related painful erection (SRPE) is a parasomnia of unknown origin characterised by penile pain, wakening the patient and possibly resulting in excessive daytime sleepiness [1, 3]. We present the case of a 65-year-old technician with negative medical history. He was a “matiné idol” with many sexual relationships all his adult life, although he had wife and children. His awakenings with torturing penile pain during night-time erections started at the age of 55 years; the pain gradually increased and the frequency of unpleasant erections increased to 3–5/night. The penile pain spread over the lower body. As soon as he was fully awake, erection and pain disappeared together; in later years, however, the pain persisted. To get rid of pains he increased sexual activity, but with no success. Then he sought medical help. Two and three years after his problems started, uro-surgical operations were performed for the ill-localised pain: first a trans-urethral-prostatic-resection (although he had no urinary retention); then an operation for anal fissure. In 1999 he was referred to our sleep-clinic. His physical status, laboratory tests, and whole spine MRI were normal. He was severely depressed. Whole-night-polysomnography (Brainquick System III MS–40) including phallography, demonstrated disrupted night-sleep with three erections 1–7 minutes after the onset of REM-sleep phases (Table). Erections lasting 3–8 minutes were accompanied by arousal and full awakening from REM sleep, then they abruptly disappeared. Repeated tests showed similar findings. Brain MRI revealed a neurovascular compression on the antero-lateral surface of the left hypothalamus by the left posterior cerebral artery (Figure).
Treatment with metoprolol, clozapine and clonazepam was ineffective. After a transitory improvement on clomipramin his complaints reappeared. Our patient’s symptoms covered the criteria of SRPE. In our opinion, uro-surgical procedures, probably performed because of pain only, show the danger of unrecognised parasomnia leading to poorly justified operations. In SRPE the pain could result from erectile hyper-activity during REM-sleep, due to central overdrive. Our patient’s increased daytime sexual activity seems to support this theory; however, the short duration of his night-time erections does not. The theory that SRPE is a psycho-somatic disorder [2] is supported by the depression of our patient, but preservation of sleep-related erections also in vegetative-state-patients [9] and independence from pre-sleep sexual arousal [11] make it improbable. The anterior-hypothalamus is implicated in the control of reproductive behaviour [7]. Lesion of the medial preoptic area in rats eliminates copulations; while its stimulation induces erections and removes descending inhibition of penile reflexes [10]. Rats with this lesion exhibit non-contact erections near receptive females although copulatory behaviour is compromised. The bed nucleus of the stria-terminalis [8] has a critical role in the regulation of non- contact erections, related to olfactory impulses. Copulations with the lesion of this nucleus are not disrupted once initiated; however, non-contact erections disappear [10]. Also the lateral-preoptic-region is identified as a centre of non-contact erections [10]. A bilateral lesion selectively eliminates REM-sleep-related erections in rat while copulatory behaviour is preserved [10]. As sexual functions are phylogenetically ancient,we hypothesise that the same brain-areas are involved in the regulation of erections in rat and man. Consequently we assume that the lateral preoptic area may be involved in the pathophysiology of SRPE also in humans. The experimental data led us to perform brain MRI,which revealed a neurovascular compression of the lateral preoptic area. The definition of neurovascular compression syndromes is that a brain vessel adversely placed induces irritation or a lesion of affected structures leading to dysfunction. It is acknowledged that vascular compression of the trigeminal nerve leads to trigeminal neuralgia. We suggest that in this case the posterior cerebral artery clearly compressing the inferior basal forebrain stimulates and /or damages it, leading to SRPE. References1. American Sleep Disorders Association (ASDA) (1997) ICSD – International Classification of sleep disorders, revised. Diagnostic and coding manual. Rochester,Minnesota American Sleep Disorders Association 2. Calvet U (1999) Painful nocturnal erection. Sleep Med Rev 3: 47–57 3. Ferini-Strambi L, Oldani A, Zucconi M, et al. (1996) Sleep-related painful erections: clinical and polysomnographic features. J Sleep Res 5: 195–197 4. Fischer C, Gross J, Zilch J (1965) A cycle of penile erections synchronous with dreaming (REM) sleep.Arch Gen Psychiatry 12: 29–45 5. Karacan I, Hursch CJ, William RI, Thornby JI (1972) Some characteristics of nocturnal penile tumescence in young adults.Arch Gen Psychiatry 26: 351–356 6. Lavie P (1990) Penile erections in a patient with nearly total absence of REM: a follow-up study. Sleep 13: 276–278 7. Meston CM, Penny F, Frohlich MA (2000) The Neurobiology of Sexual Function.Arch Gen Psychiatry 57: 1012–1030 8. Nauta WJH, Feirtag M (1986) Fundamental Neuroanatomy. Freeman and Company,New York 9. Oxenberg A, Arons E, Sazbon L, Mizrahi A, Radwan (2000) Sleep-Related Erections in Vegetative state Patients. Sleep 23: 953–958 10. Schmidt MH, Valatx JL, Sakai K, Fort P, Jouvet M (2000) Role of the lateral preoptic area in sleep-related erectile mechanisms and sleep generatio 11. Ware JC, Hirshkowitz M, Thornby J, Salis P, Karacan I (1997) Sleep-related erections: absence of change following presleep sexual arousal. J Psychosom Res 42: 547–553 |