In vitro
IN VITRO functional assays
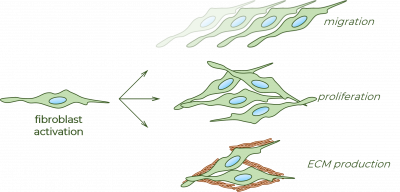
Recent antifibrotic drug development projects target the inhibition of fibroblasts, the main effector cells of fibrosis. In our in vitro experiments, (near-)high-throughput functional assays – suitable for drug screening – are used to invesigate the behavior of fibroblasts.
Migration
Due to their unique actin filament network, fibroblasts bear with enhanced migration capacity. As a consequence of tissue damage or inflammation, various cytokines, chemokines, growth factors are released, which attract fibroblast to the site of the injury. Using transient agarose spot (TAS) migration assay, the motility of fibroblasts can be investigated constitutively for several days.
This method is based on graphical analysis of cell free area size, determining the kinetic of gap closure.
Proliferation
Active fibroblasts are characterized by increased proliferation and decreased apoptosis rate. The increasing amount of fibroblasts form the main cellular part of the connective tissue. Using MTT assay, endogenous and induced proliferation of fibroblasts can be measured. In parallel, the activity of LDH in the supernatant of cells can be also determined, which indicate the extent of cell death.
These methods are based on the colorimetric measurement of substrate-product conversion by intracellular enzymes.
ECM production
Beside their increased migration and proliferation ability, fibroblasts are also the main source of the non-cellular part of the connective tissue – extracellular matrix (ECM) proteins, including collagens and fibronectin, as well. Using SiriusRed assay, collagen deposition of fibroblast can be measured.
This method is based on the colorimetric measurement of a well-known histological staining, internalized into the triple helix of collagen proteins accumulated surrounding the fibroblasts.
In vivo
IN VIVO EXPERIMENTS
Experimental rodent models of fibrosis are unavoidable elements of antifibrotic drug development. In our in vivo experiments, we use numerous models inducing fibrosis in various organs to test the antifibrotic effect of drug candidates. Beside of its efficacy, the possible toxic effect of the examined compound is also investigated by monitoring various parameters, such as the condition, body weight and behavior of the animals.
Renal fibrosis induced by unilateral ureteral obstruction (UUO)
In this model, the left ureter of the mice is ligated using surgical thread. After a few days, the accumulating urine in the renal pelvis induces hydronephrosis and consequent renal fibrosis. The experiment is usually terminated at the 7th or 14th day, when tissue samples are harvested. The extent of renal fibrosis is determined by numerous histological- and molecular biological measurements, evaluating the protein and mRNA expression of fibroblast-related markers and extracellular matrix elements.
Gastrointestinal fibrosis induced by dextran sodium sulfate (DSS)
In this model, a severe colitis is induced by treating mice with a chemical reagent, DSS dissolved in their drinking water. After a few days, gastrointestinal symptoms appear and worsen until the 7th day, when DSS-treatment is terminated and mice are offered pure water during the regeneration phase. Body weight change and disease activity is monitored daily by a complex scoring system. The experiment is usually terminated at the 19th day, when tissue samples are harvested. The extent of intestinal fibrosis is determined by colon weight/length ratio and by numerous histological and molecular biological measurements, evaluating the protein and mRNA expression of fibroblast-related markers and extracellular matrix elements.
Lung fibrosis induced by bleomycin
In this model, mice are treated with multiple intraperitoneal injection of bleomycin, which is an anticancer drug, inducing oxidative-stress mediated cell death in cell types with increased metabolic rate, such as cancer cells. However, bleomycin induces sensitivity to oxygen in healthy cell types as well, especially in lung epithelial cells, resulting in pulmonary inflammation and fibrosis. The experiment is usually terminated at the 21st day after the first injection of bleomycin, when tissue samples are harvested. The extent of pulmonary fibrosis is determined by lung weight and by numerous histological and molecular biological measurements, evaluating the protein and mRNA expression of fibroblast-related markers and extracellular matrix elements.
Peritoneal fibrosis induced by chlorhexidine digluconate
In this model, mice are treated with multiple intraperitonal injection of chlorhexidine digluconate (CG) solution, diluted in ethanol. CG induces profibrotic processes in the peritoneal tissue leading to mesothelial-to-mesenchymal transition (MMT), fibroblast activation and abnormal transport capacity. The extent of peritoneal fibrosis is determined by quantifying submesothelial thickness, measuring peritoneal permeability and by numerous molecular biological measurements, evaluating the protein and mRNA expression of fibroblast-related markers and extracellular matrix elements.